Role of teleradiology in the interpretation of ultrasound images acquired in the emergency setting
- Авторлар: Kalyanpur A.1, Mathur N.2
-
Мекемелер:
- Teleradiology Solutions
- Image Core Lab
- Шығарылым: Том 5, № 2 (2024)
- Беттер: 231-242
- Бөлім: Original Study Articles
- ##submission.dateSubmitted##: 15.12.2023
- ##submission.dateAccepted##: 24.01.2024
- ##submission.datePublished##: 20.09.2024
- URL: https://jdigitaldiagnostics.com/DD/article/view/624586
- DOI: https://doi.org/10.17816/DD624586
- ID: 624586
Дәйексөз келтіру
Аннотация
BACKGROUND: Teleradiology has become an important tool in emergency medicine, particularly in the interpretation of emergency ultrasonography. In emergency situations, where time is essential, rapid diagnosis and treatment can mean the difference between life and death. Teleradiology is an innovative alternative to augment the staffing and fill the gaps of onsite radiology personnel in emergency departments or during off-hours.
AIM: To assess the effectiveness/impact of teleradiology in emergency ultrasound interpretation.
MATERIALS AND METHODS: A retrospective study was performed in a cohort of 33,616 patients from 86 hospitals across the USA between January and December 2022. The study involved radiological interpretations of 37,253 ultrasound images acquired in the emergency setting by American Board Certified Radiologists empaneled by a teleradiology service provider, headquartered in Bangalore, India.
RESULTS: The proposed telehealth model provided timely and quality reporting of 37,253 scans of patients with a mean turnaround time of 35.71 min (95% confidence interval 35.50–35.91).
CONCLUSION: This study demonstrates that a structured telesonography program with defined protocols for image capture, transmission, and clinical communication can allow for successful immediate reporting of ultrasound data in the emergency care setting.
Негізгі сөздер
Толық мәтін
BACKGROUND
Teleradiology epitomizes healthcare innovation and efficient healthcare delivery and represents a success story within the wider field of telemedicine [1]. This rapidly expanding field involves the transmission of radiological images from one location to another for interpretation by a radiologist [2]. It is an indispensable tool in emergency medicine, significantly improving patient care. Prompt interpretation and reporting of radiologic examinations by a teleradiologist in the evaluation of specific emergent complaints render it a significant part of the emergency medicine diagnostic paradigm [3].
Emergency cases within emergency departments (EDs) have notably increased over the past couple years, which was strongly associated with population growth and further heightened during the COVID pandemic [4]. EDs are also vulnerable to crowding during catastrophic disasters, such as earthquakes, tsunamis, cyclones, and urban flooding [5]. According to the National Hospital Ambulatory Medical Care Survey: 2020, the total number of visits to EDs of the hospitals in the US was 131.3 million [6], which is a matter of concern. In India, the NITI Aayog (2021) reported that 16% of all patients presenting to a health facility have emergency and injury cases, accounting for 19%–36% of admissions in district hospitals annually [5]. In addition, a report released by the Department of Emergency Medicine, AIIMS, on Emergency and Injury Care at Secondary and Tertiary level centers in India revealed that the number of beds available at EDs to cater to emergency cases, represents only 3%–5% of the total beds available in the country [7]. With a yearly rise in the number of people who visit EDs, nearly half of all EDs operate at or exceeding their capacity. This trend is very concerning and must be addressed [8]. Moreover, there is a shortage of physicians, particularly radiologists, i.e., approximately 22,000 radiologists for a large population of over 1.2 billion, resulting in a skewed ratio of 1:100,000 [9]. Considering the severity of trauma, stroke, and other critical illness of patients presenting to the EDs, diagnostic and treatment delays can lead to serious consequences for patients. Thus, timely and accurate interpretation of patients’ imaging is pivotal. However, the availability of in-house trained radiologists is limited in EDs, particularly after working hours or on holidays. The challenge is to work toward efficiency and quality despite the rising workload and the shortage of medical personnel [10]. Under such circumstances, teleradiology is an obvious alternative to augment, assist, and fill in the gaps of the onsite radiology personnel in meeting the rising demand for imaging in trauma and acute illnesses in an emergency setting with a limited radiology workforce [8].
Emergency ultrasonography (USG) is a diagnostic imaging technique that utilizes high-frequency sound waves to create images of internal organs and structures [12]. It is a fast and noninvasive method of evaluating various clinical conditions, including trauma, abdominal and pelvic pain, appendicitis, cholecystitis, acute kidney dysfunction, abscess, complications of pregnancy, complications of organ transplantation [13]. Doppler USG is a real-time imaging technology that plays a pivotal role in emergency radiology for quick evaluation of vascular conditions and blood flow. It allows the identification of potentially fatal conditions such as deep vein thrombosis, arterial blockage, and insufficient organ perfusion. Diagnosing vascular damage in trauma cases facilitates timely performance of surgical intervention [14].
The major benefit of teleradiology in emergency sonography is not only the ability to provide timely diagnosis and treatment but also to offer adequate after-hour and specialist coverage including support for onsite ultrasound technologists/sonographers. Teleradiology in emergency USG can also lead to cost reductions for hospitals and patients [15]. Several studies have documented the benefits of teleradiology for patients [1, 11, 16, 17], and the present study aimed to evaluate the benefits of teleradiology in emergency ultrasound interpretation.
The advent of digital imaging technologies, picture archiving and communication systems (PACS), radiology information systems (RIS), high-speed Internet connections, and artificial intelligence have further improved the value proposition of teleradiology in providing timely radiological services under emergency settings, even to remote and underserved areas [11, 18, 19]. Moreover, stringent service-level agreements between the hospital and the teleradiology service guarantee a very short reporting turnaround time (TAT), which is advantageous to the patient and the attending emergency physician. The standard for clinical service in emergency care has thus been enhanced thanks to teleradiology [1, 20].
AIM STUDY
This retrospective study aimed to evaluate the role of teleradiology in USG performed on a cohort of patients in the emergency setting.
MATERIALS AND METHODS
Study Design
A retrospective study enrolled a cohort of 33,616 patients from 86 hospitals across the USA between January and December 2022. The study involved analysis of radiological ultrasonogram interpretations performed in the emergency setting by American Board Certified Radiologists empanelled by a teleradiology service provider, headquartered in Bangalore, India. DICOM static images and cine-series of the ultrasound images of the patients were uploaded onto the telereporting workflow platform “RADspa,” a cloud-based RIS/PACS system over a high-speed Internet connection. In addition to uploading the images, the technologists at the hospitals also provided observations in a worksheet submitted along with the images. The worksheet was typically a combination of an annotated graphic image with measurements and free text comments. The images (static images and cine-series) and worksheets were reviewed by the radiologists, and the reports were transmitted back to the hospitals over the same workflow platform, as well as conveyed verbally/telephonically in cases with critical findings. Other information, such as prior images and reports, patient clinical and surgical history records, are also uploaded to the RIS so that they are available to the radiologists along with the images.
A distribution of studies for different procedures performed in the emergency setting was analyzed. The mean reporting TAT from the time when the DICOM images of emergency ultrasound studies were received in the worklist up until the reports were uploaded in RADspa or verbally communicated to the referring physician was calculated.
Eligibility Criteria
The study included patients who had registered in the EDs of the hospitals and undergone USG.
Study Duration
The study enrolled a cohort of 33,616 patients from 86 hospitals across the USA between January and December 2022.
Ethical Review
This retrospective study was approved by the institutional review board.
RESULTS
Study Subjects
A total of 37,253 ultrasound scans of 33,616 patients from 86 hospitals across the US were evaluated.
Primary Findings
The hospitals were categorized based on the bed count and number of images received (Table 1).
Table 1. Distribution of hospitals according to bed count and imaging
Hospital bed count | Number of hospitals | Number of cases |
Small hospitals (<100 beds) | 22 | 1,621 |
Medium-size hospitals (100–499 beds) | 54 | 29,692 |
Large hospitals (≥500 beds) | 7 | 981 |
Imaging centers | 3 | 4,959 |
Total | 86 | 37,253 |
Among all hospitals under study, 28 had in-house technologists to perform ultrasound scans for the patients, out of which 4 had on-call technologists on weekends. In addition, 51 hospitals had on-call technologists, whereas in one hospital, radiology residents reported ultrasound cases. In six hospitals, technologists do not perform ultrasound scans after 11 pm.
In a teleradiology practice, technologists communicate in three ways and provide brief descriptions of the cases to the teleradiologists. Technologists create worksheets with case observations and upload these in the RADspa either as pdf or jpeg file, may convert them into DICOM, or may write down their comments or notes directly into the textbox provided in RADspa. In this study, out of 37,253 ultrasound scans, the technologists had provided notes for 27,138 (72.84%) cases, and for the remaining cases, worksheets were attached.
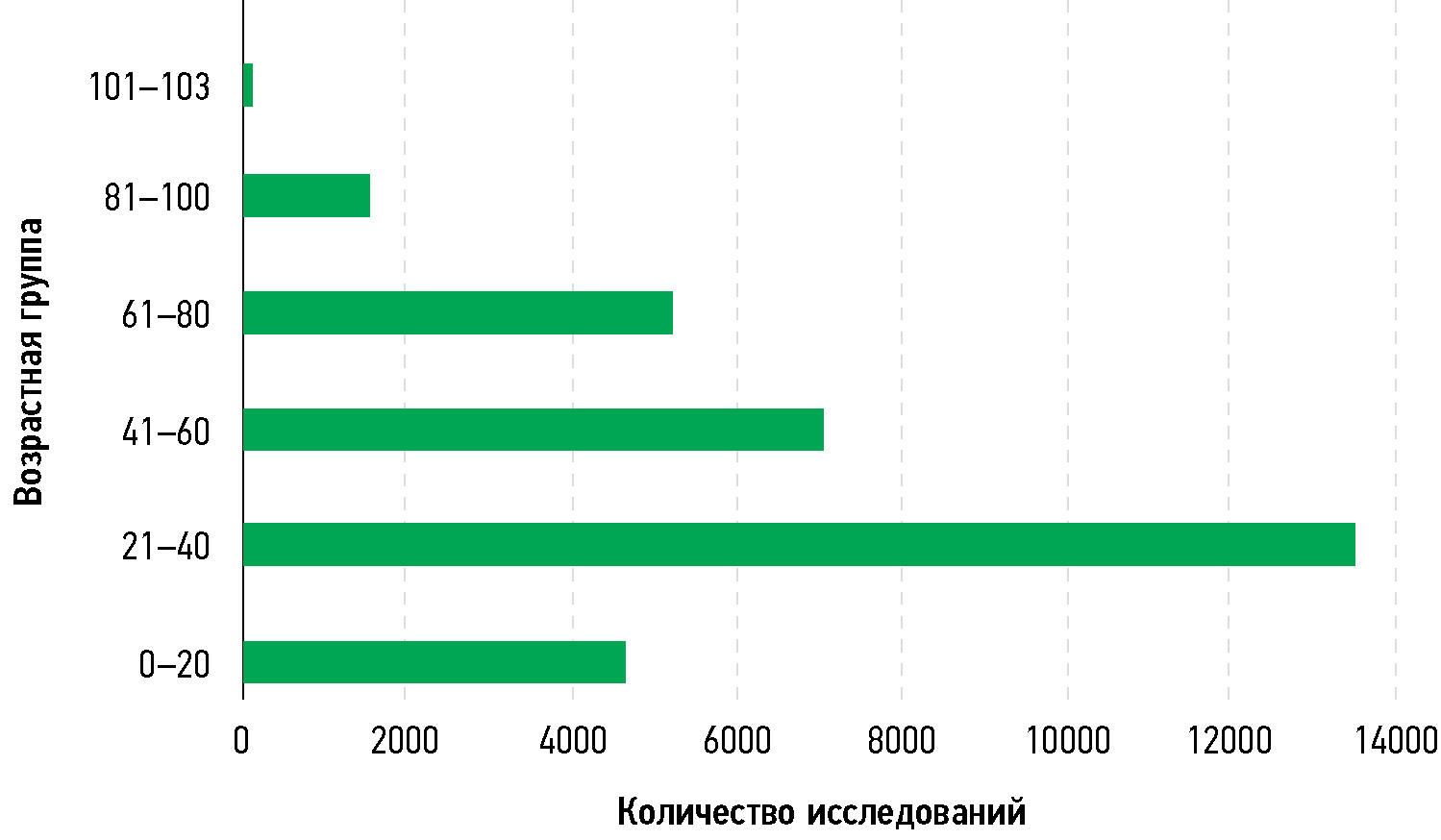
Demographic information, such as the sex and age of the patients, was also loaded into the cloud-based server. Out of 33,616 patients in this study, 70.56% were women and 29.44% were men. The mean age of the patients was 40.95 (95% confidence interval, 40.73–41.17) years. The group aged 21–40 years accounted for the maximum number of patients (Fig. 1).
Fig. 1. Age group categorization of the patients.
To help in making diagnosis and treatment decisions, ultrasound scans of different body parts were performed (Table 2). Among the ultrasound procedures performed, lower and upper extremity USG comprised 26.28% (n = 9,792); abdomen, 18.62% (n = 6,937); obstetrics, 17.41% (n = 6,488), and pelvis, 15.62% (n = 5,820). Out of 33616 patients, 9496 had followed up with computed tomography.
Table 2. Distribution of studies for different procedures
Procedures | Number of cases |
Venous Doppler (lower/upper extremity) | 9,792 |
Abdomen | 6,937 |
Obstetrics biophysical profile | 6,488 |
Pelvis (non-pregnant female)/transvaginal /endovaginal | 5,820 |
Gallbladder/right upper quadrant/appendix/liver/right lower quadrant | 3,965 |
Scrotal/testicular/scrotum Doppler | 1,977 |
Renal/retroperitoneal | 1,393 |
Breast | 184 |
Carotid Doppler | 152 |
Neck | 115 |
Soft Tissue | 79 |
Intussusception | 69 |
Carotid Duplex | 60 |
Groin | 35 |
Chest | 29 |
Urinary bladder | 24 |
Extracranial arteries, both | 19 |
Fistula graft | 18 |
Head | 18 |
Thyroid | 18 |
Kidney transplantation | 12 |
Other procedures | 49 |
Teleradiology services were provided to the patients under different clinical situations. Patient clinical texts were categorized based on the presenting symptoms, and a systems-based approach was employed (Fig. 2). The majority of the presenting symptoms were categorized as reproductive (35%), gastrointestinal (31%), cardiovascular (9%), and musculoskeletal (6%). Other categories, shown in Fig. 2, make up smaller proportions of the presenting symptoms of the overall study cohort.
Fig. 2. Distribution of cases based on clinical presentation and symptoms using a systems-based approach.
Cine-series of 4,025 patients were also uploaded into the cloud server for interpretation by teleradiologists. Out of 4,025 cine-series, 1,731 (43%), 1,048 (26.03%), and 655 (16.27%) were performed for issues related to the reproductive, gastrointestinal, and cardiovascular systems, respectively (Fig. 3).
Fig. 3. Distribution of cases with cine-series using a systems-based approach.
In this study, 1,262 patients had undergone Doppler, of which 569 patients who had clinical history of scrotal or testicular pain, swelling, torsion and hydrocele underwent scrotal Doppler. Further, 497 patients having cysts, suspected ovarian torsion, pelvic pain, cramps, vaginal bleeding during pregnancy, post-menopausal bleeding, and lower abdominal pain had undergone pelvic Doppler. In addition, 152 patients with numbness, vertigo, slurred speech, syncope, CVA, transient ischemic stroke and stenosis underwent carotid Doppler. Twenty-eight patients with abnormal gallbladder, liver or spleen, hepatic encephalopathy, liver failure, cirrhosis, hepatic vein thrombosis, and liver transplantation underwent liver Doppler, and 16 cases with renal failure underwent renal Doppler (Fig. 4).
Fig. 4. Distribution of cases for Doppler ultrasound.
The mean reporting TAT for all emergency ultrasound studies was 35.71 min (95% CI, 35.50–35.91).
Additional Findings
All ultrasound scans were peer-reviewed under a quality assurance program to assess diagnostic accuracy and clinical performance. Out of 37,253 ultrasound scans, 99.9% of the studies showed accurate and concurrent interpretations, and 39 (0.1%) studies showed discrepancies. Among these 39 cases, 24 had nonclinically significant discrepancies, whereas 15 were clinically significant ones.
DISCUSSION
Emergency care is the provision of immediate interventions required to prevent death and disability, wherein delays over hours may worsen prognoses or reduce the efficacy of care [21]. With the development of emergency radiology as a distinct radiology specialty, a unique set of expertise is essential to diagnose patients with critical illnesses or trauma promptly and accurately [11]. Teleradiology is an innovative solution that enables quick interpretation of imaging and accurate diagnosis of patients with critical injuries or illnesses requiring immediate resuscitation, intensive care, or emergent surgery, allowing emergency physicians to make informed decisions about patient care and treatment plans. Further, the proposed emergency teleradiology model, where night-to-day teleradiology services are leveraged, i.e., emergency scans performed at night in the USA can be reported from India during the day by appropriately certified radiologists, and vice versa, could be a front-line driver in healthcare. At present, emergency radiology subspecialty training or dedicated emergency radiology positions are not available. Several emergency radiology and medicine societies, namely, the Society of Emergency Radiology, European Society of Emergency Radiology, American Society of Emergency Radiology, Society for Emergency Medicine India, and Indian Society for Trauma and Acute Care have been founded to promote the exchange of best practices in the area and enable integration of clinical care and imaging [22].
This retrospective study involves the evaluation and interpretation of imaging of emergency cases transmitted from 86 hospitals across the USA. According to the information obtained from the Annual Survey of Hospitals, the total staffed beds in all US hospitals is 919,649 [23]. The hospitals are broadly categorized based on the bed count as small (<100 beds), medium (100–499 beds), and large (≥500 beds) hospitals. In this study, the hospitals were categorized based on the bed count and number of imaging studies received (Table 1). The majority of the studies (79.7%) were transmitted by 54 medium hospitals, and 13% were transmitted by three imaging centers. This study demonstrates that hospitals of any size may benefit from telesonography.
Telesonography may be effectively practiced in either model (in-house or on-call technologist). Out of 86 hospitals, 28 had in-house technologists who helped in establishing better communication of results compared with hospitals having on-call technologists.
Of all ultrasound scans, 17,333 (35%) were from patients presenting reproductive-related issues, followed by 15,653 (31%) with gastrointestinal/biliary issues, 4,295 (9%) with vascular problems, and 2,952 (6%) with musculoskeletal-related issues that required immediate medical attention. Other smaller categories included 1,531 studies of skin-related cases, 1,398 of urinary system-related problems, 365 of neurologic issues, and 280 of respiratory-related problems (Fig. 2). Thus, teleradiology in USG covers the entire gamut of organ systems and clinical presentations to address emergent clinical needs.
The mean TAT is the interval from when the DICOM images of emergency ultrasound studies were received in the worklist to the time the reports were uploaded in RADspa or verbally communicated to the referring physician/results were sent to hospitals. The mean reporting TAT for all emergency ultrasound studies was 35.71 min (95% CI, 35.50–35.91). Szabo et al. reported a mean TAT of 58.27 min for USG within the ED of a hospital system with in-house radiologists. In the present study, the mean TAT using teleradiology is quite reasonable and satisfactory compared with the mean TAT for USG by other published studies with onsite radiologists, thus displaying the effect of teleradiology on patient care in the emergency setting [24].
In addition, this study demonstrates that static images of standard views accompanied by the sonographer’s worksheets are adequate for the interpretation of ultrasound studies via telesonography in most cases. Additional cine sequences can be used in complex cases to provide additional details.
With reference to the communication of findings, in critical cases requiring immediate patient management, referring physicians were informed either by direct telephonic communication with the radiologist or the call center team of the teleradiology service provider [25]. In this study, a total of 752 calls were made to communicate with the hospitals. Out of these calls, 49 direct calls were made between the radiologist and the referring physician, and 70 calls were made by the support staff to relate positive findings and 47 calls to communicate negative findings. In addition, 619 calls were performed for the verbal communication of important findings to physician assistants at hospitals who ensured further actions.
A peer review plays an indispensable role in a radiology interpretation QA program. A QA program is the most common method for assessing diagnostic accuracy and clinical performance. In this study, a very high accuracy (99.9%) was observed during the peer review. Only 39 (0.1%) studies showed discrepancies. Among these 39 cases, 24 were nonclinically significant discrepancies, whereas 15 were clinically significant ones. In a study by Iyer et al. (2013), 85.9% of the cases had concurrent interpretations. Some discrepancies analyzed during peer review were under-reading, faulty reasoning, failure to provide appropriate differential diagnosis, overcall, typographical error, failure to consult before imaging studies, and failure to suggest further imaging or follow-up.
CONCLUSION
Teleradiology has become an important tool in emergency medicine where time is essential, and rapid diagnosis and treatment can mean the difference between life and death. Many EDs do not have a radiologist on site to interpret ultrasound images, which can lead to diagnostic and treatment delays. Under such circumstances, the deployment of teleradiology services can be a game changer owing to its ability to provide quick and accurate diagnoses, further leading to the expedient and safer disposition of patients. This study demonstrates that a structured telesonography program with defined protocols for image capture, transmission, and clinical communication can allow for the successful immediate reporting of ultrasound examinations in the emergency care setting. The findings of the proposed telehealth model seek to provide a platform for constructing a similar telesonography model in developing countries.
ADDITIONAL INFORMATION
Funding source. This study was not supported by any external sources of funding.
Competing interests. The authors declare that they have no competing interests.
Authors’ contribution. All authors made a substantial contribution to the conception of the work, acquisition, analysis, interpretation of data for the work, drafting and revising the work, final approval of the version to be published and agree to be accountable for all aspects of the work.
A. Kalyanpur — conceptualization, formal analysis and investigation, writing and editing, supervision; N. Mathur — formal analysis and investigation, writing, original draft preparation.
Авторлар туралы
Arjun Kalyanpur
Teleradiology Solutions
Email: arjun.kalyanpur@telradsol.com
ORCID iD: 0000-0003-2761-7273
MD
Үндістан, BangaloreNeetika Mathur
Image Core Lab
Хат алмасуға жауапты Автор.
Email: neetika.mathur@imagecorelab.com
ORCID iD: 0009-0002-8884-2060
PhD
Үндістан, BangaloreӘдебиет тізімі
- Kalyanpur A. The role of teleradiology in emergency radiology provision. Radiol Manage. 2014;36(3):46–49.
- Burute N, Jankharia B. Teleradiology: The Indian perspective. Indian Journal of Radiology and Imaging. 2009;19(1):16–18. doi: 10.4103/0971-3026.45337
- Michalke JA. An overview of emergency ultrasound in the United States. World J Emerg Med. 2012;3(2):85–90. doi: 10.5847/wjem.j.issn.1920-8642.2012.02.001
- Misra A, Yadav DC, Kole T. Emergency care in India beyond 75 years of independence — problems and solutions. J Glob Health. 2023;13:03015. doi: 10.7189/jogh.13.03015
- National Hospital Ambulatory Medical Care Survey: 2020 Emergency Department Summary Tables [Internet]. US: National Center for Health Statistics. Available from: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2020-nhamcs-ed-web-tables-508.pdf
- Perotte R, Lewin GO, Tambe U, et al. Improving Emergency Department Flow: Reducing Turnaround Time for Emergent CT Scans. AMIA Annu Symp Proc. 2018;2018:897–906.
- Agrawal A, Khandelwal N. Nucleating emergency radiology specialization in India. Emerg Radiol. 2016;23(2):101–103. doi: 10.1007/s10140-016-1381-6
- Abdolrazaghnejad A, Banaie M, Safdari M. Ultrasonography in Emergency Department; a Diagnostic Tool for Better Examination and Decision-Making. Adv J Emerg Med. 2018;2(1):e7. doi: 10.22114/AJEM.v0i0.40
- Nicola R, Dogra V. Ultrasound: the triage tool in the emergency department: using ultrasound first. Br J Radiol. 2016;89(1061):20150790. doi: 10.1259/bjr.20150790
- Islam SN, Deka N, Hussain Z. Role of Doppler Ultrasound in Assessing the Severity of Peripheral Arterial Diseases of the Lower Limb. J Med Ultrasound. 2021;29(4):277–280. doi: 10.4103/JMU.JMU_137_20
- Kalyanpur A, Meka S, Joshi K, Somashekaran Nair HT, Mathur N. Teleradiology in Tripura: Effectiveness of a Telehealth Model for the Rural Health Sector. International Journal of Health Technology and Innovation. 2022;1:7–12. doi: 10.60142/ijhti.v1i02.36
- Agrawal A. Emergency Teleradiology-Past, Present, and, Is There a Future? Front Radiol. 2022;2:866643. doi: 10.3389/fradi.2022.866643
- Kalyanpur A, Weinberg J, Neklesa V, et al. Emergency radiology coverage: technical and clinical feasibility of an international teleradiology model. Emerg Radiol. 2003;10(3):115–118. doi: 10.1007/s10140-003-0284-5
- Agrawal A, Agrawal A, Pandit M, Kalyanpur A. Systematic survey of discrepancy rates in an international teleradiology service. Emerg Radiol. 2011;18(1):23–29. doi: 10.1007/s10140-010-0899-2
- Chandramohan A, Krothapalli V, Augustin A, et al. Teleradiology and technology innovations in radiology: status in India and its role in increasing access to primary health care. The Lancet Regional Health — Southeast Asia. 2023;23. doi: 10.1016/j.lansea.2023.100195
- Thrall JH. Teleradiology Part I. History and Clinical Applications. Radiology. 2007;243(3):613–617. doi: 10.1148/radiol.2433070350
- Duarte ML, Dos Santos LR, Iared W, Peccin MS. Telementored ultrasonography: a narrative review. Sao Paulo Med J. 2022;140(2):310–319. doi: 10.1590/1516-3180.2020.0607.R2.15092021
- Bergquist HB, Burkholder TW, Muhammad Ali OA, Omer Y, Wallis LA. Considerations for service delivery for emergency care in low resource settings. African Journal of Emergency Medicine. 2020;10:S7–S11. doi: 10.1016/j.afjem.2020.07.002
- Agrawal A, Khandelwal N. Nucleating emergency radiology specialization in India. Emerg Radiol. 2016;23(2):101–103. doi: 10.1007/s10140-016-1381-6
- Fast Facts on U.S. Hospitals [Internet]. US: American Hospital Association. c2024. Available from: https://www.aha.org/statistics/fast-facts-us-hospitals
- Szabo I, Zag L, Takács I, et al. Quantile regression and an application: performance improvement of an emergency department in Eastern Europe. Hungarian Statistical Review. 2020;3(1):60–76. doi: 10.35618/hsr2020.01.en060
- Honig SE, Honig EL, Babiarz LB, et al. Critical findings: timing of notification in neuroradiology. AJNR Am J Neuroradiol. 2014;35(8):1485–1492. doi: 10.3174/ajnr.A3918
Қосымша файлдар