Delphi method to determine a list of questionnaire-assessed parameters in the follow-up of patients with inflammatory bowel disease
- Авторлар: Shumskaya Y.F.1, Akhmedzyanova D.A.1, Mnatsakanyan M.G.2, Kolosova K.Y.2, Tashchyаn O.V.2, Yurazh M.V.2, Reshetnikov R.V.1
-
Мекемелер:
- Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies
- The First Sechenov Moscow State Medical University
- Шығарылым: Том 4, № 4 (2023)
- Беттер: 481-491
- Бөлім: Original Study Articles
- ##submission.dateSubmitted##: 11.07.2023
- ##submission.dateAccepted##: 31.08.2023
- ##submission.datePublished##: 15.12.2023
- URL: https://jdigitaldiagnostics.com/DD/article/view/545997
- DOI: https://doi.org/10.17816/DD545997
- ID: 545997
Дәйексөз келтіру
Аннотация
BACKGROUND: Patients with inflammatory bowel disease often require lifelong follow-up by a clinician. Telemedicine monitoring is a promising area of such healthcare services, often based on the evaluation of patients’ remote questionnaire results by a medical practitioner.
AIM: To define, using the Delphi method, a list of questionnaire-assessed parameters for monitoring and treating patients with IBD.
MATERIALS AND METHODS: The study was conducted in three stages. An electronic survey form was created to collect information, ensuring that the respondent’s experience was included when completing the survey. In the first stage, respondents answered an open-ended question about what parameters assessed by questionnaires should be monitored in patients with IBD. In the second stage, participants answered the same question but selected any number of items from a list. In the third stage, the responses were analyzed. The primary endpoint was a consensus on each parameter, defined as >75% respondent agreement.
RESULTS: The study had 15 participants, 13.3% of whom were male. Of all respondents, 46% worked in an outpatient setting, whereas 54% worked in an inpatient setting. Their ages ranged from 25 to 53 years, with 53% of the participants having 1–4 years of experience and 47% having 17–29 years of experience. None of the parameters reached a 75% agreement level based on the results of the first stage. In the second stage, respondents reached a consensus on 72% of the parameters. No relationship was found between respondents’ age, sex, years of experience, or job settings and responses in the first and second stages.
CONCLUSIONS: The final list of parameters recommended for evaluation during the monitoring and treatment of patients with IBD included abdominal pain, frequency of defecation and stool quality, presence of pathological stool impurities, body temperature, joint/muscle pain, sleep quality, anxiety, depression, work capacity for employed/ability to attend lessons for students, energy and quantity of vigor, fixation on the disease, patients’ general evaluation of their quality of life, and treatment adherence.
Толық мәтін
BACKGROUND
Inflammatory bowel diseases (IBDs), particularly ulcerative colitis and Crohn’s disease, are major public health concerns because of their severity, comorbidities, and high treatment costs. IBDs frequently affect not only health but also quality of life, deteriorating patients’ physical and mental well-being and limiting their social capabilities [1]. The incidence of IBD is steadily increasing both globally [2] and in Russia [3], with 55.4% of patients with ulcerative colitis and 48.5% of patients with Crohn’s disease were 21 to 40 years old [4]. Because of the recurring nature of IBD, most patients require lifelong monitoring; however, no unified protocol has been established for the outpatient management of these patients during remission.
Telemedicine is a promising approach to the outpatient management of patients with IBD. Patients under remote follow-up have a significantly better quality of life and seek medical attention less frequently than patients receiving standard treatment [5]. However, with remote follow-up, the question of what must be assessed arises.
The assessment of critical laboratory parameters such as C-reactive protein and fecal calprotectin is undeniably important. However, in addition to IBD activity parameters, other factors are crucial for quality of life, such as psychological status, which are not assessed in routine practice.
Questionnaires are a convenient and relevant method for assessing a patient’s condition. They provide the clinician with the necessary information, such as the clinical activity of IBD or compliance, without requiring high costs or time commitments. Most studies have assessed disease activity and associated quality of life; however, other studies have less frequently assessed the overall quality of life, depression severity, adherence to drug therapy, and patient satisfaction with medical care [5]. Moreover, few studies have assessed visceral sensitivity [6] and the effect of the disease on work productivity [7, 8] and sexual activity [9] in patients with IBD. In addition, researchers did not explain why they chose specific endpoints. As a result, the lack of consensus on the parameters assessed by questionnaires prevents their standardized use managing patients with IBD.
PURPOSE
This study aimed to use the Delphi method to assess the expert opinions of gastroenterologists to determine a list of questionnaire-assessed parameters in the follow-up of patients with IBD.
MATERIALS AND METHODS
Between May and June 2023, gastroenterologists treating IBD were invited to participate in a survey to achieve a consensus on the inclusion/exclusion of various parameters in patient assessment during treatment and follow-up. The Delphi method was used to obtain a collective opinion with reasonable level of validity and reliability and explore areas outside existing knowledge [10]. Before the study commenced, a literature review on the use of questionnaires in the assessment of patients with IBD was performed. Following the literature review, the areas assessed by Russian and foreign authors were determined (Table 1).
Table 1. Response options for multiple-choice questions in the second stage of the survey
Area | Proposed parameter |
Clinical activity of the disease | Abdominal pain |
Defecation frequency and stool form | |
Pathological admixtures in the feces | |
Body temperature | |
Joint/muscle pain | |
Psychological status | Emotional state: anxiety |
Emotional state: mood | |
Sleep quality | |
Body image perception (negative/positive) | |
Quality of life | Patient global assessment of quality of life |
Quality of communication | |
Quality of sexual life | |
Ability to work/study | |
Others | Anxious attitude toward the disease |
Visceral sensitivity | |
Energy level | |
Patient satisfaction with medical care |
Participants were chosen at random by convenience sampling. No consensus on the sample size for studies using the Delphi method, guidelines, or a clear definition of a “small” or “large” sample was reached [11, 12]. In this study, the sample size was determined according to R.B. Akins et al., who demonstrated that the results of the Delphi method in a group of experts in the studied area are stable with 15 –23 participants [13].
The study included three stages. Information was collected using an electronic survey form using Yandex Forms.
Stage I
To participate in the survey, all participants had to specify their work experience as a gastroenterologist. In stage I, all participants answered the following open-ended questions:
“What aspects of life and health, in your opinion, should be assessed in a patient with inflammatory bowel disease, both during treatment of an attack and during follow-up in remission?”
Respondents could proceed to the next stage of the survey after filling out the answer field. Stage I answers were stratified into four:
- Clinical activity assessment
- Psychological status assessment
- Quality of life assessment
- Others
Stage II
In stage II, the participants had to select items from the list. The question was as follows:
“Select the items from the list below that you believe are crucial to assess in a patient with inflammatory bowel disease, both during treatment of an attack and during follow-up in remission.”
The possible answers presented in Table 1 were derived from a literature review using PubMed. Original studies and systematic reviews that assessed the efficacy of treatment in patients with IBD were analyzed, and the endpoints of these studies were identified. No restrictions were set on the number of the selected items.
Upon completion of stage II, the survey participants were invited to optionally supplement their answers to stage I question (without showing respondents the text of their previous answers).
Stage III
In stage III, the responses were analyzed. The primary endpoint was the consensus on the inclusion of patient assessment parameters in the final list. The consensus on a specific parameter was reached when >75% of respondents choose the parameter [14].
The software and language R 4.2.0 were used for data analysis. The Shapiro–Wilk test was employed to check the normality of the distribution. Variables with normal distribution are presented as mean ± standard deviation. Variables with non-normal distribution are presented as median and interquartile range. The correlation between variables was assessed by calculating Spearman’s or Pearson’s rank correlation coefficient, depending on the type of distribution.
After the study, the respondents were interviewed, using the following questions:
- Which was easier to answer: an open-ended question or a multiple-choice question?
- Why do you think some items did not receive enough votes? (This question included items that received <75% of the votes)
RESULTS
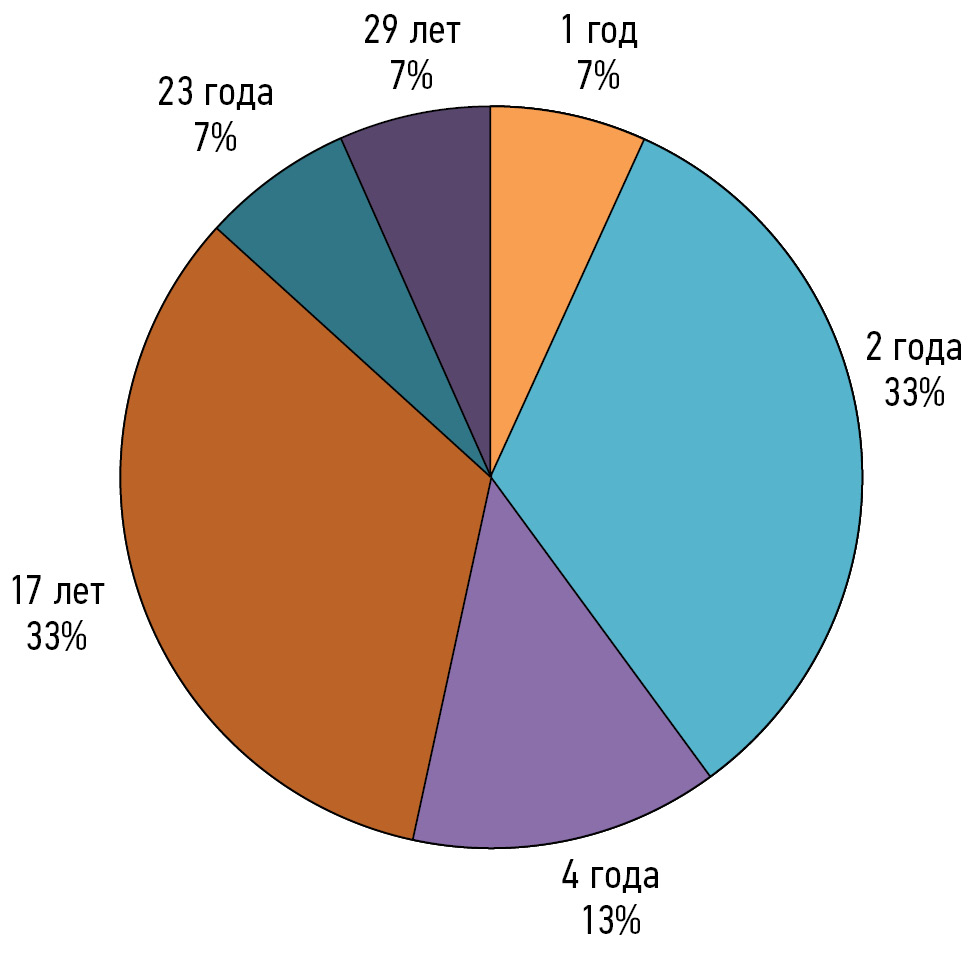
The study included 15 respondents, 13.3% of whom were men. The mean age of the participants was 36.6 ± 9.9 years, ranging from 25 to 53 years. Outpatient physicians accounted for 46% of all respondents, whereas hospital physicians accounted for 54%. None of the respondents withdrew from the study. The distribution of participants according to work experience is presented in Fig. 1.
Fig. 1. Distribution of the study participants according to their work experience as gastroenterologists.
According to the results of stage I, in which study participants must answer an open-ended question, no obvious overlaps were found in the answers because of the free format. After categorizing the answers, none of the categories attained the level of agreement (Fig. 2).
Fig. 2. Study results (first stage). The red dotted line indicates 75% of the respondents.
Based on the results of stage I, the “compliance” parameter was added to the possible answers in stage II (in addition to the items listed in Table 1). The results of stage II differed from those of stage I for each respondent: the number of questionnaire-assessed parameters (median number of parameters, 4 [3; 5.5] and 16 [13.5; 17] for stages I and II, respectively) increased.
Fig. 3. Study results (second stage). The red columns indicate parameters that received <75% of the responses.
In the correlation analysis, no link was found between the age, sex, work experience, and place of work (outpatient clinic/hospital) of respondents and their answers during stages I and II.
Participants were interviewed after receiving the results of stage II. Compared with answering a multiple-choice question, answering an open-ended question was more challenging for 100% of the respondents. In total, 27% of the participants responded when asked why some items did not receive enough votes. Each of them emphasized that the quality of sexual life and communication in patients with IBD is frequently influenced by factors other than the disease. According to the respondents, body image perception is unrelated to the disease and does not warrant assessment by a gastroenterologist. Respondents also did not believe that satisfaction with medical care was a parameter that clinicians should monitor in all patients with IBD. Regarding visceral sensitivity, respondents agreed on the importance of assessing this parameter in some patients whose symptoms cannot be explained solely by the clinical course of IBD and who may benefit from the addition of a functional component.
DISCUSSION
The study generated a final list of parameters recommended for assessment during the treatment and follow-up of patients with IBD, which included the following:
- Abdominal pain
- Defecation frequency and stool form
- Pathological admixtures in the feces
- Body temperature
- Joint/muscle pain
- Sleep quality
- Emotional state: anxiety
- Emotional state: mood
- Ability to work/study
- Energy level
- Anxious attitude toward the disease
- Patient global assessment of quality of life
- Compliance
This list was compiled after a two-stage survey of gastroenterologists. Two approaches were used to collect information in this study: an open-ended question and a multiple-choice question. In the first scenario, no consensus could be reached on any of the categories; however, in the second scenario, respondents agreed on 72% of the parameters. This could be due to the simplicity of stage II: during the interview, respondents stated that answering a multiple-choice question was easier and more convenient for them.
Furthermore, no correlation was found between the characteristics of the survey participants, such as sex, age, work experience, and place of work (outpatient clinic or hospital), and their answers during stages I and II.
Our findings support the use of the Delphi method, which offers equal opportunities to survey participants and allows for the concealment of expertise and skill level to prevent the authority pressure that is unavoidable in face-to-face discussions. In this study, clinicians with minimal experience had the same perceptions of follow-up strategies as their more experienced colleagues. There may be other scenarios in which the consensus is not as strong; in such cases, a fresh look at the topic under discussion by young specialists may lead to a more objective decision.
According to foreign literature, health-related quality of life, disability/ability to work, and disease activity are the key questionnaire-assessed parameters in patients with IBD [15]. In this study, these areas were also included in the final list. The first five parameters selected by the participants (abdominal pain, defecation frequency and stool form, pathological admixtures in feces, body temperature, and joint/muscle pain) are related to assessing the clinical activity of IBD. The ability to work/study and patient global assessment of quality of life were also selected by >90% of the respondents.
Furthermore, the final list included parameters that assessed the emotional state, such as sleep quality, anxiety, and mood. Given the high incidence of anxiety and depression symptoms in patients with IBD [16], assessing these parameters will surely provide valuable information to researchers and clinicians.
Assessing energy levels in patients with IBD is also critical, given the subjective and complex nature of asthenic syndrome in these patients [17]. We believe that this parameter must be used by clinicians and researchers, depending on the clinical setting or study endpoints.
Compliance assessment in patients with IBD is also important, given the often lifelong drug therapy, including immunosuppressants. Because compliance is one of the treatment goals [18], its assessment is critical for clinicians and researchers.
In a systematic review, Pang et al. used disease-related quality of life, inflammation activity, and remission rate as primary endpoints. Secondary endpoints included overall quality of life, depression, compliance, and satisfaction with medical care [5]. However, the researchers did not explain why these specific parameters were selected as outcomes. Our study presents a consensus list of questionnaire-assessed parameters in the follow-up of patients with IBD.
Advantages and limitations
Clinicians from various backgrounds were invited to participate in the study, which has advantages and disadvantages. Analysis of a large proportion of young participants brings a fresh viewpoint; however, these participants have limited practical experience. Participation of both outpatient and inpatient care workers allows for a wider range of perspectives.
Further studies
A larger-scale survey with more gastroenterologists from various Russian regions appears to be a logical and necessary extension of this study. Professionals discussing scientific challenges together allow us to address current issues and propose new solutions [19]. Guidelines detailing a pool of questionnaires in areas determined by consensus will be developed as part of the practical implementation of the study findings.
ADDITIONAL INFORMATION
Funding source. This article was prepared by the authors as a part of the research and development effort titled “Scientific evidence for using telemedicine-based models and methods for organization and delivery of medical care” (Russian United scientific information system No. 123031400008-4) in accordance with the order of the Moscow Healthcare Department No. 1196 dated December 21, 2022 “On approval of state assignments funded by means of allocations from the budget of the city of Moscow to the state budgetary (autonomous) institutions subordinate to the Moscow Healthcare Department, for 2023 and the planned period of 2024 and 2025”.
Competing interests. The authors declare that they have no competing interests.
Authors’ contribution. All authors made a substantial contribution to the conception of the work, acquisition, analysis, interpretation of data for the work, drafting and revising the work, final approval of the version to be published and agree to be accountable for all aspects of the work. Yu.F. Shumskaya, D.A. Akhmedzynova, K.Yu. Kolosova, M.V. Yurazh ― writing the original draft; Yu.F. Shumskaya, O.V. Tashchyan ― data curation, investigation; M.G. Mnatsakanyan, R.V. Reshetnikov, Yu.F. Shumskaya ― conceptualization, study design; Yu.F. Shumskaya, R.V. Reshetnikov — data curation.
Авторлар туралы
Yuliya Shumskaya
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies
Хат алмасуға жауапты Автор.
Email: shumskayayf@zdrav.mos.ru
ORCID iD: 0000-0002-8521-4045
SPIN-код: 3164-5518
Ресей, Moscow
Dina Akhmedzyanova
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies
Email: AkhmedzyanovaDA@zdrav.mos.ru
ORCID iD: 0000-0001-7705-9754
SPIN-код: 6983-5991
Ресей, Moscow
Marina Mnatsakanyan
The First Sechenov Moscow State Medical University
Email: mnatsakanyan_m_g@staff.sechenov.ru
ORCID iD: 0000-0001-9337-7453
SPIN-код: 2015-1822
MD, Dr. Sci. (Med.), Professor
Ресей, MoscowKsenia Kolosova
The First Sechenov Moscow State Medical University
Email: kolosova_k_yu@staff.sechenov.ru
ORCID iD: 0000-0001-7641-2755
MD, Cand. Sci. (Med.)
Ресей, MoscowOlga Tashchyаn
The First Sechenov Moscow State Medical University
Email: olgatash1@rambler.ru
ORCID iD: 0000-0001-6759-6820
MD, Cand. Sci. (Med.)
Ресей, MoscowMarta Yurazh
The First Sechenov Moscow State Medical University
Email: yurazh_m_v@staff.sechenov.ru
ORCID iD: 0000-0002-4459-7481
SPIN-код: 4872-7130
Ресей, Moscow
Roman Reshetnikov
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies
Email: reshetnikov@fbb.msu.ru
ORCID iD: 0000-0002-9661-0254
SPIN-код: 8592-0558
Cand. Sci. (Phys.-Math.)
Ресей, MoscowӘдебиет тізімі
- Romberg-Camps MJL, Bol Y, Dagnelie PC, et al. Fatigue and health-related quality of life in inflammatory bowel disease. Inflammatory Bowel Diseases. 2010;16(12):2137–2147. doi: 10.1002/ibd.21285
- Windsor JW, Kaplan GG. Evolving Epidemiology of IBD. Current Gastroenterology Reports. 2019;21(8. doi: 10.1007/s11894-019-0705-6
- Khalif IL, Shapina MV. Inflammatory bowel disease treatment in Eastern Europe. Current Opinion in Gastroenterology. 2017;33(4):230–233. doi: 10.1097/mog.0000000000000370
- Belousova EA, Shelygin YuA, Achkasov SI, et al. Clinical and Demographic Features and Treatment Approaches for Inflammatory Bowel Diseases (Crohn’s Disease, Ulcerative Colitis) in the Russia. The Primery Results of the Analysis of the National Register. Koloproktologia. 2023;22(1):65–82. (In Russ) doi: 10.33878/2073-7556-2023-22-1-65-82
- Pang L, Liu H, Liu Zh, et al. Role of Telemedicine in Inflammatory Bowel Disease: Systematic Review and Meta-analysis of Randomized Controlled Trials. Journal of Medical Internet Research. 2022;24(3):e28978. doi: 10.2196/28978
- Trieschmann K, Chang L, Park S, et al. The visceral sensitivity index: A novel tool for measuring GI-symptom-specific anxiety in inflammatory bowel disease. Neurogastroenterology & Motility. 2022;34(9). doi: 10.1111/nmo.14384
- Jackson BD, Con D, Gorelik A, et al. Examination of the relationship between disease activity and patient-reported outcome measures in an inflammatory bowel disease cohort. Internal Medicine Journal. 2018;48(10):1234–1241. doi: 10.1111/imj.13937
- Thomas PWA, Broeder N, Derikx M, et al. Impact of Biological Therapies and Tofacitinib on Real-world Work Impairment in Inflammatory Bowel Disease Patients: A Prospective Study. Inflammatory Bowel Diseases. 2022;28(12):1813–1820. doi: 10.1093/ibd/izac002
- Chen B, Zhou B, Song G, et al. Inflammatory bowel disease is associated with worse sexual function: a systematic review and meta-analysis. Translational Andrology and Urology. 2022;11(7):959–973. doi: 10.21037/tau-22-190
- Murphy MK, Black NA, Lamping DL, et al. Consensus development methods, and their use in clinical guideline development. Health Technology Assessment. 1998;2(3):I–IV. doi: 10.3310/hta2030
- Williams PL, Webb C. The Delphi technique: a methodological discussion. Journal of Advanced Nursing. 1994;19(1):180–186. doi: 10.1111/j.1365-2648.1994.tb01066.x
- Wilhelm W. Alchemy of the Oracle: the Delphi technique. The Delta Pi Epsilon Journal. 2001;43:6–26.
- Akins RB, Tolson H, Cole BR. Stability of response characteristics of a Delphi panel: application of bootstrap data expansion. BMC Medical Research Methodology. 2005;5(1). doi: 10.1186/1471-2288-5-37
- Diamond IR, Grant RC, Feldman BM, et al. Defining consensus: A systematic review recommends methodologic criteria for reporting of Delphi studies. Journal of Clinical Epidemiology. 2014;67(4):401–409. doi: 10.1016/j.jclinepi.2013.12.002
- Andel EM, Koopmann BDM, Crouwel F, et al. Systematic Review of Development and Content Validity of Patient-reported Outcome Measures in Inflammatory Bowel Disease: Do We Measure What We Measure? Journal of Crohn’s and Colitis. 2020;14(9):1299–1315. doi: 10.1093/ecco-jcc/jjaa057
- Barberio B, Zamani M, Black CJ, et al. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: a systematic review and meta-analysis. The Lancet Gastroenterology & Hepatology. 2021;6(5):359–370. doi: 10.1016/s2468-1253(21)00014-5
- Halpin SJ, Ford AC. Prevalence of Symptoms Meeting Criteria for Irritable Bowel Syndrome in Inflammatory Bowel Disease: Systematic Review and Meta-Analysis. American Journal of Gastroenterology. 2012;107(10):1474–1482. doi: 10.1038/ajg.2012.260
- Yu N, Basnayake C, Connell W, et al. Interventions to Improve Adherence to Preventive Care in Inflammatory Bowel Disease: A Systematic Review. Inflammatory Bowel Diseases. 2022;28(8):1177–1188. doi: 10.1093/ibd/izab247
- Vinogradova IA, Nizovtsova LA, Omelyanskaya OV. Innovative strategic session in the scientific activity of the Center for Diagnostics and Telemedicine. Digital Diagnostics. 2023;3(4):414–420. (In Russ) doi: 10.17816/DD111833
Қосымша файлдар