二尖瓣粘液瘤
- 作者: Vishniakova M.V.1, Abramenko A.S.1, Vishniakova M.V.1, Shumakov D.V.1
-
隶属关系:
- Moscow Regional Research and Clinical Institute
- 期: 卷 3, 编号 1 (2022)
- 页面: 64-70
- 栏目: 临床病例及临床病例的系列
- ##submission.dateSubmitted##: 07.02.2022
- ##submission.dateAccepted##: 07.04.2022
- ##submission.datePublished##: 24.04.2022
- URL: https://jdigitaldiagnostics.com/DD/article/view/100281
- DOI: https://doi.org/10.17816/DD100281
- ID: 100281
如何引用文章
详细
原发性心脏肿瘤是一种极为罕见的疾病,根据各种来源,其在人群中的患病率为0.0017–0.03%。
在大多数情况下,心脏肿瘤为良性,其中一半以上为心脏粘液瘤。影响瓣叶的粘液瘤是一种非常罕见的病理现象。1934年首次描述了这种类型的变化。大多数情况下,心脏粘液瘤位于卵圆窝附近的房间隔水平。粘液瘤的典型症状之一是狭窄的腿和不平整的表面,这会导致栓塞的风险。超声心动图和磁共振成像目前是疑似心脏肿块的选择法。在此类非典型的肿瘤定位的情况下,必须与心脏瓣膜上的赘生物和乳头状弹力纤维瘤进行鉴别诊断。
介绍了一名老年患者的病例,主诉喘息,左胸刺痛,心律失常,此患的病史包括吸引性肺炎,食管胃吻合术,食道摘除术。患者检查发现阵发性心房颤动(阵发外)、慢性心力衰竭、动脉高血压。患者的临床资料不具感染性心内膜炎特征,瓣膜上有赘生物。超声心动图和多螺旋计算机断层扫描在二尖瓣后叶的心房表面进行快速对比增强,显示额外的体积形成 5-9 毫米,圆形,轮廓明显不均匀,与瓣叶一起移位进入心房收缩期左心室腔。在Fiesta-CINE模式下,在修改后的两室和四室投影中获得了肿块的最佳可视化。患者在体外循环下接受了肿块的切除,并进行了二尖瓣成形术。肿块的组织学检查揭示了粘液瘤的特征性形态情况。术后期间一切顺利。
全文:
绪论
原发性心脏肿瘤是一种极为罕见的疾病,根据各种来源,其在人群中的患病率为0.0017–0.03%[1, 2]。在大多数情况下,心脏肿瘤为良性,其中一半以上为心脏粘液瘤[3–7]。
粘液瘤被认为起源于心内膜中多能间充质细胞的残余碎片。大多数情况下,心脏粘液瘤位于卵圆窝附近的房间隔水平。粘液瘤的典型特征之一是狭窄的柄和不规则的表面。这使得这种类型的肿瘤有发生栓塞的风险。
病例报告
T.患者, 64岁,入院时主诉呼吸短促,左胸刺痛,心律失常。病史显示了吸入性肺炎,食管异物取出术与食管胃成形术。
物理、实验室和仪器检查结果
检查发现阵发性房颤(阵发性以外) ,IIA、II功能级慢性心力衰竭,以及三级动脉高血压。
超声心动图显示二尖瓣轻度功能不全,以及位于蒂上二尖瓣后瓣形成,尺寸达9 mm。
对于形成的详细描述,胸部器官的状态评估,冠状动脉的状态评估,在General Electric Optima MR450w GEM 1,5 T设备上对Philips iCT 256片进行多螺旋CT扫描,同时进行心电同步和心脏磁共振成像(MRI)。
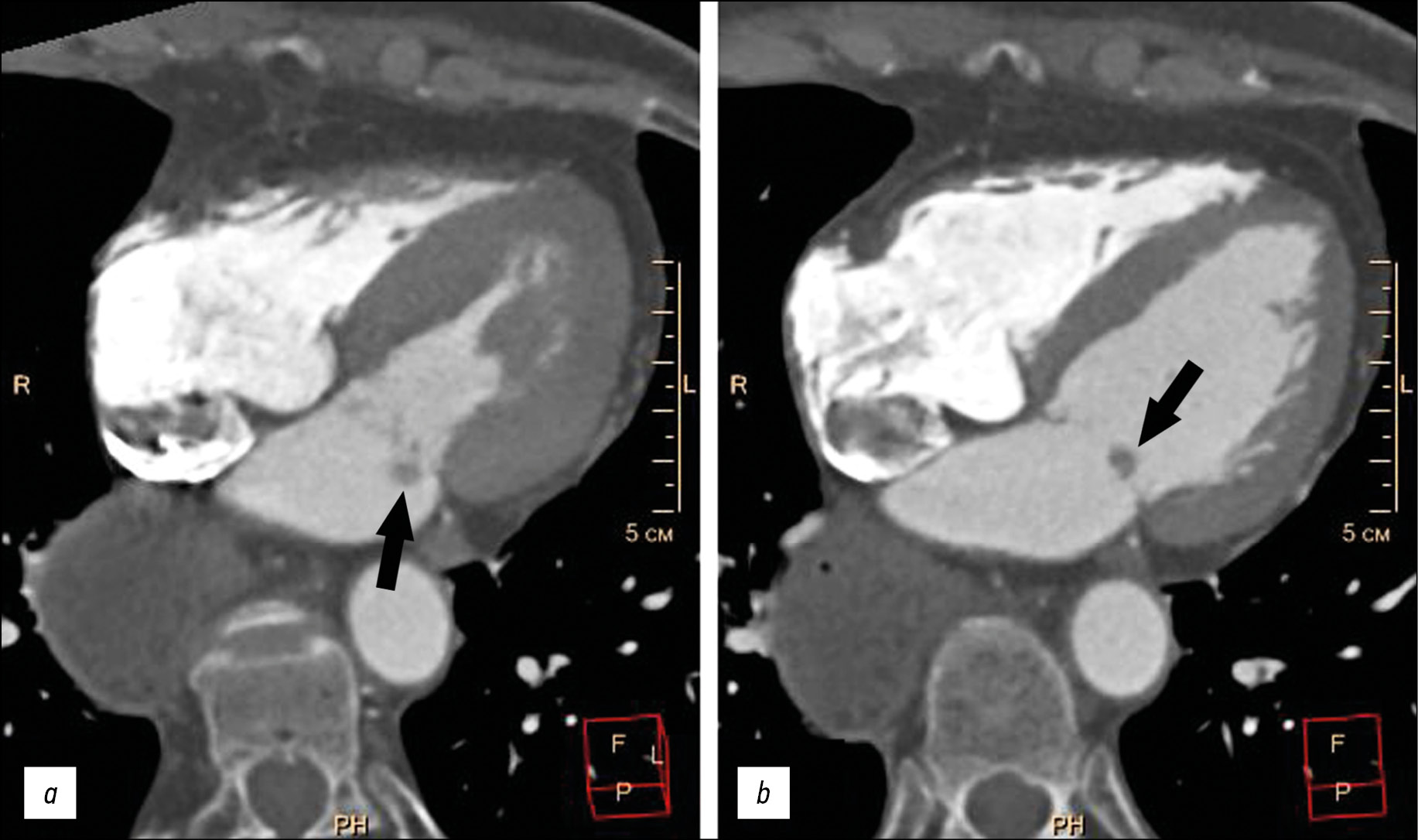
在计算机断层扫描期间,没有额外的体积形成和炎症浸润区域的肺组织被发现。被切除的食道床的胃腔被确定为在该水平没有病理肿块。检查时没有发现冠状动脉的明显狭窄。在二尖瓣后瓣心房表面,可以看到额外的5–9 mm的体积形成,形状圆形,轮廓明显不均匀,与二尖瓣瓣一起进入左心室腔进入心房收缩(图 1)。
图 1胸部多层计算机断层扫描,心脏四腔平面重建,动脉造影阶段:a——左心室收缩期;b——左心室舒张期。二尖瓣后瓣上的额外圆形结构(黑色箭头)。
在心脏MRI中,经过一系列概述和轴向胸部扫描后,在标准轴(两腔、四腔长轴,切片厚度为8 mm,相交间隔为0 mm)进行一系列Fiesta-CINE功能研究。由于肿瘤形成的小尺寸,在心脏MRI的标准投影上显示肿瘤是困难的。在Fiesta-CINE模式下,在修改后的两室和四室投影中获得了肿块的最佳可视化(图 2)。
图 2心脏的磁共振成像,双腔投影:a——左心室收缩期;b——左心室舒张期。二尖瓣后瓣上的额外肿块(黑色箭头)。
证实了二尖瓣后瓣位于左心房一侧,有一个大小为5×8 mm的小圆形。为了获得肿块的组织特征,使用T2 SS、FSE、FS--T2 VI脉冲序列进行了增强前和增强后的对比度增强研究,其中血液和脂肪组织的信号被抑制,对比度后图像为PS MDE(PSIR),TI 250 ms。对照剂(钆喷酸葡胺注射液)以0.2 ml/kg患者体重的剂量给予。
延迟增强后,与T1-VI序列相比,信号增强( 图 3)。
图 3心脏的磁共振成像,双腔投影:a——原生T1-VI系列,TSE;b——对比后T1-VI系列,TSE。二尖瓣后瓣上的额外肿块(白色箭头)。
患者在体外循环下接受了肿块的切除,并进行了二尖瓣成形术。术后无显示并发症。
肿块的组织学检查揭示了粘液瘤的特征性形态情况。
讨论
尽管粘液瘤是心脏最常见的原发肿瘤,但这种疾病的病例数量在一般人群中非常少。影响瓣叶的粘液瘤是一种非常罕见的病理现象。1934年首次描述了这种类型的变化[8]。
目前国外文献所描述的确切病例数尚不清楚,但在粘液瘤中这种定位的大约患病率不超过1.5%[9, 10]。
超声心动图检查和MRI是目前在怀疑心脏体积形成的情况下选择的方法。对于这种不典型的肿瘤定位,与心脏瓣膜赘生物和乳头状纤维弹性瘤的鉴别诊断是必要的[5, 6]。
赘生物多位于二尖瓣心房表面。这在我们的临床病例中得到证实,但影像学技术已经发现了肿块蒂,更多的是提示是一个肿块。在延迟对比度增强的MRI中,植被的特点是不均匀的对比度积聚。这使得我们很难区分植被和肿块[11, 12],然而,在本文的病例中,缺乏瓣膜上植被的感染性心内膜炎的临床资料。
心脏乳头样弹性纤维瘤是第二常见的良性原发肿瘤。肿瘤的特征是小(通常小于15 mm),圆形,短蒂。典型的定位是二尖瓣的心房表面或主动脉瓣的主动脉表面[2, 13]。
结论
尽管使用了现代影像技术,但在描述的临床病例中没有发现心脏粘液瘤的特殊征象。然而,由于存在肿瘤性质的移动性肿块,需要进行手术治疗,之后的组织学检查导致组织学诊断为极为罕见的局部肌瘤。
ADDITIONAL INFORMATION
Funding source. The article had no sponsorship.
Competing interests. The authors declare that they have no competing interests.
Authors’ contribution. All authors made a substantial contribution to the conception of the work, acquisition, analysis, interpretation of data for the work, drafting and revising the work, final approval of the version to be published and agree to be accountable for all aspects of the work.
Consent for publication. Written consent was obtained from the patient for publication of relevant medical information and all of accompanying images within the manuscript.
作者简介
Marina V. Vishniakova
Moscow Regional Research and Clinical Institute
编辑信件的主要联系方式.
Email: cherridra@mail.ru
ORCID iD: 0000-0003-3838-636X
SPIN 代码: 1137-2991
MD, Dr. Sci. (Med)
俄罗斯联邦, 61/2, Shepkina street, Moscow,129110Alexander S. Abramenko
Moscow Regional Research and Clinical Institute
Email: a.s.abramenko@gmail.com
ORCID iD: 0000-0002-6286-2162
SPIN 代码: 9743-3001
Научный сотрудник отделения лучевой диагностики
俄罗斯联邦, 61/2, Shepkina street, Moscow,129110Mariya V. Vishniakova
Moscow Regional Research and Clinical Institute
Email: cherridra@list.ru
ORCID iD: 0000-0002-2649-4198
SPIN 代码: 7748-1831
MD, Dr. Sci. (Med)
俄罗斯联邦, 61/2, Shepkina street, Moscow,129110Dmitry V. Shumakov
Moscow Regional Research and Clinical Institute
Email: cherridra@mail.ru
ORCID iD: 0000-0003-4204-8865
SPIN 代码: 2545-2978
MD, Dr. Sci. (Med), Corresponding Member of the Russian Academy of Sciences
俄罗斯联邦, 61/2, Shepkina street, Moscow,129110参考
- Centofanti P, Di Rosa E, Deorsola L, et al. Primary cardiac tumors: early and late results of surgical treatment in 91 patients. Ann Thorac Surg. 1999;68(4):1236–1241. doi: 10.1016/s0003-4975(99)00700-6
- Hoey ET, Shahid M, Ganeshan A, et al. MRI assessment of cardiac tumours: part 1, multiparametric imaging protocols and spectrum of appearances of histologically benign lesions. Quant Imaging Med Surg. 2014;4(6):478–488. doi: 10.3978/j.issn.2223-4292.2014.11.23
- Zheltovsky YV, Batekh VI, Podkamenny VA, et al. Diagnosis and treatment with a heart mix. Acta Biomedica Sci. 2017;2(6):21–26. (In Russ).
- Lam KY, Dickens P, Chan AC. Tumors of the heart. A 20-year experience with a review of 12,485 consecutive autopsies. Arch Pathol Lab Med. 1993;117(10):1027–1031.
- Li X, Chen Y, Liu J, et al. Cardiac magnetic resonance imaging of primary cardiac tumors. Quant Imaging Med Surg. 2020;10(1):294–313. doi: 10.21037/qims.2019.11.13
- Aggeli C, Dimitroglou Y, Raftopoulos L, et al. Cardiac masses: the role of cardiovascular imaging in the differential diagnosis. Diagnostics. 2020;10(12):1088. doi: 10.3390/diagnostics10121088
- Kallstrom E, Kallus E, Erbe K, et al. Differentiation of left atrial myxomas by multimodality imaging. J Diagnostic Med Sonography. 2020;36(1):52–63. doi: 10.1177/8756479319872153
- Jaleski TC. Myxoma of the heart valves: report of a case. Am J Pathol. 1934;10(3):399–406.
- Wold LE, Lie JT. Cardiac myxomas: a clinicopathologic profile. Am J Pathol. 1980;101(1):219–240.
- Yoon JH, Kim JH, Sung YJ, et al. Cardiac myxoma originating from the anterior mitral valve leaflet. J Cardiovasc Ultrasound. 2011;19(4):228–231. doi: 10.4250/jcu.2011.19.4.228
- Rajiah P, Moore A, Saboo S, et al. Multimodality imaging of complications of cardiac valve surgeries. Radio Graphics. 2019;39(4):932–956. doi: 10.1148/rg.2019180177
- El Ouazzani J, Jandou I, Christophe Thuaire I. Thrombus or vegetation? Importance of cardiac MRI as a diagnostic tool based on case report and literature review. Ann Med Surg (Lond). 2020;60:690–694. doi: 10.1016/j.amsu.2020.12.007
- Anand S, Sydow N, Janardhanan R. Papillary fibroelastoma diagnosed through multimodality cardiac imaging: a rare tumour in an uncommon location with review of literature. BMJ Case Rep. 2017;2017:bcr2017219327. doi: 10.1136/bcr-2017-219327
补充文件