诊断能力:在主动脉瘤中使用磁共振成像的创新方法
- 作者: Kobelev E.1, Pak N.T.1, Bobrikova E.E.1, Ussov W.Y.2, Kliver E.E.1, Sirota D.A.1, Chernyavskiy A.M.1, Bergen T.A.1
-
隶属关系:
- E. Meshalkin National Medical Research Center
- Tomsk National Research Medical Center
- 期: 卷 3, 编号 3 (2022)
- 页面: 332-339
- 栏目: 临床病例及临床病例的系列
- ##submission.dateSubmitted##: 31.05.2022
- ##submission.dateAccepted##: 29.06.2022
- ##submission.datePublished##: 17.10.2022
- URL: https://jdigitaldiagnostics.com/DD/article/view/108404
- DOI: https://doi.org/10.17816/DD108404
- ID: 108404
如何引用文章
详细
本文介绍了磁共振成像在确定手术策略方面的创新应用。
作者描述了一名47岁患者的病例,该患者接受了磁共振成像,随后对主动脉瘤进行了手术治疗。与超声心动图不同,此类诊断方法可以看到整个胸主动脉,与计算机断层扫描不同,它有助于识别主动脉壁的变化。使用磁共振成像,我们能够确定切除的远心端。术后期间一切顺利。根据与心电图同步的数据,我们评估了主动脉壁的结构变化及其力学性能。值得注意的是,磁共振成像的结果与组织学检查的结果相关。
为了对主动脉瘤患者进行有效的手术治疗,必须确定血管壁的变化程度。
主动脉壁的磁共振成像是一个很有前途的诊断方向,需要在多中心研究中进一步研究。
全文:
研究现实性
对胸主动脉瘤患者应评估其手术适应症,但因合并症或生活质量差而预期寿命有限的情况除外[1]。根据最新建议,检查包括计算机断层扫描(CT)或磁共振成像(MRI)以测量主动脉直径[2-4]。
我们提出了一种新的独特方法来在胸主动脉瘤患者中使用核磁共振成像,这使我们能够确定最佳的手术策略。
病例报告
关于患者
患者,男性,47岁,根据MRI数据已接受主动脉瘤手术治疗,既往无加重因素或慢性病史。
升主动脉的动脉瘤对医生来说总是一个挑战。超声心动图检查显示升主动脉扩张至5.5 cm,无主动脉瓣反流。
仪器检查结果
患者接受了与心电图同步的主动脉MRI和心脏MRI。该检查是在带有专门线圈的1.5Т磁共振成像上进行的。使用没有对比增强的T2和T1加权图像,再使用增强的T1加权图像。在MRI扫描期间进行了对比增强的血管造影(图1)。升主动脉最大直径5.4 cm,动脉瘤近端和尾部之间的距离为9 cm;头臂干口前的主动脉直径——3.4 cm,左颈总动脉和锁骨下动脉口之间——2.4 cm,下降部分——2.3 cm。头臂干边缘到动脉瘤颅缘的距离为5.5 cm。
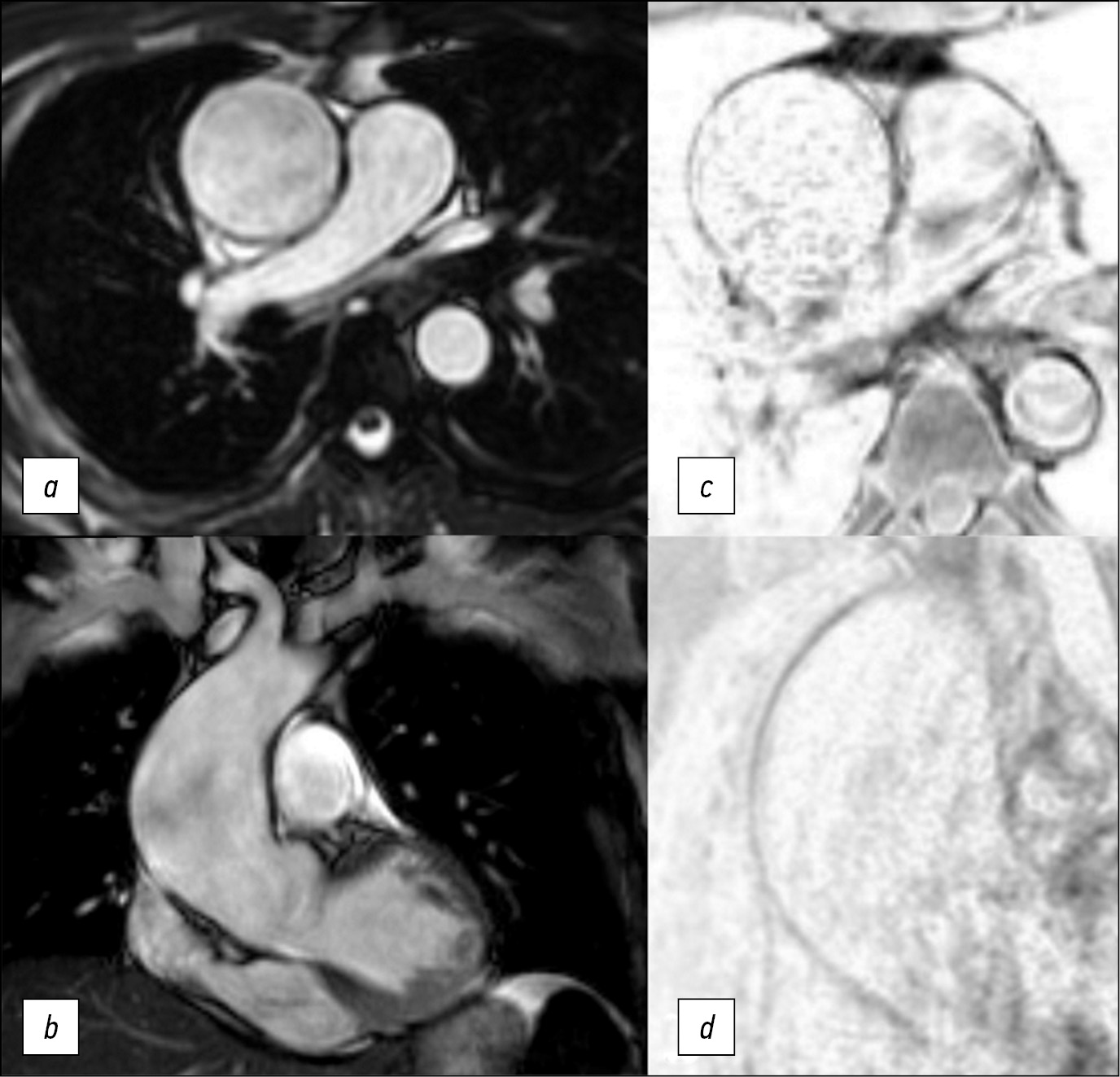
为了评估主动脉壁的弹性和收缩性,使用了在轴向和冠状投影中以稳态自由进动(steady-state free precession, SSFP)模式获得的原生图像(见图1)。
图1。在轴位(a)和冠位(b)中以SSFP模式获得的图像,在轴位(c)中以T1-SE(主动脉瘤的中间三分之一) ,在斜投影中以“黑血”模式获得的T1-SPIR(d)。主动脉壁变薄,中部更明显。
在SSFP模式下,我们能够清楚地显示出心动周期期间主动脉壁的运动和血流方向。在QFlow序列(包括导管的可视化)中进行MRI以定量估值脉搏波速度,或如需评估瓣膜的功能。升主动脉壁的厚度和血管化是通过轴位的T1加权自旋回波(T1-spin echo, T1-SE)和梯度回波(T1-gradient-echo, GRE)序列中取得照片评估的,具有光谱选择性信号抑制的T1加权序列,在“黑血”模式(图2)中的光谱饱和和反转恢复序列(Т1-spectral presaturation with inversion recovery, T1-SPIR),在T2-在轴向和倾斜投影的“黑血”模式中具有光谱抑制的加权序列。
MRI数据显示,患者升主动脉从根部扩张 至9 cm长,最大直径为5.5 cm。动脉瘤定位区域的主动脉壁均匀变细,中部更为明显,搏动减弱,有运动障碍迹象,从动脉瘤囊边缘到头臂干主动脉壁完整不超过3 cm(见图2),主动脉直径在此水平不超过3.5 cm。还应该注意患者的二瓣叶型主动脉瓣。
图2。对比增强磁共振血管造影,动脉期,屏气,斜投影,主动脉3D重建(a); 在升主动脉瘤远端边缘的“黑血”模式下轴位的T1-SPIR(b);在斜投影中的头臂干口的前面(c)。完整的主动脉壁(箭头),手术治疗后胸主动脉的计算机断层扫描血管造影(d)。
根据现代建议[1,2,4],患者需要手术治疗。未检测到胸主动脉壁及其主要分支的近端部分的解剖、增厚和血管增生。主要分支口的解剖结构是典型的。
诊断、治疗
最初,计划在头臂干孔口前直接应用夹子,但根据核磁共振成像的结果调整了手术方法。考虑到动脉瘤远端的主动脉壁病变的普遍性,决定在循环停止和前向单侧脑灌注的情况下进行干预。值得注意的是,随着主动脉壁的切除和病理变化,在术后早期和后期都可能出现并发症。在这个病案中,患者接受了升主动脉和主动脉弓的冠状动脉上修复术,并形成了半弓型远端吻合。
手术治疗后,患者接受了胸主动脉CT血管造 影(见图2)。术后图像显示,对比主动脉腔的直径没有扩张,也没有内漏的现象。
将MRI数据与术中活检标本(切除的主动脉壁)的组织学检查结果进行比较,揭示了主动脉壁识别变化的对应关系。根据宏观研究资料,切除的主动脉壁的厚度在远端和近端边缘 为2.0-3.0 mm,在动脉瘤体的内侧部分(包括远端边缘的部分)为1.0-1.5 mm。
对动脉瘤近端和远端段以及远端切除边缘2 cm的切片进行微观研究,发现中间层广泛破坏,弹性纤维粘液样水肿,弹性膜皱襞平滑。在一些靠近血管外膜的区域,出现中度扩散性血管周围淋巴样浸润的迹象,主动脉壁部分血管的管腔闭塞。在内膜下发现了具有泡沫细胞质的巨噬细胞的局灶性聚集,不突出于表面之上(图3)。
图3。动脉瘤体的近端(a,b)和中间(c)部分。弥漫性血管周围淋巴浸润。切除的主动脉壁的远端部分(d) 。所有图像均显示弹性纤维的破坏,粘液水肿、弹性膜皱襞平滑。
基于组织学检查结果的诊断:非特异性继发性低活动性血管炎,主动脉弹性膜中间层退化。升主动脉瘤。主动脉粥样硬化,脂斑阶段。
结论
与CT扫描不同,MRI允许研究主动脉壁的结构和机械特性,测量其直径并确定最佳手术策略。
ADDITIONAL INFORMATION
Funding source. The work was carried out within the state assignment of the Ministry of Health of the Russian Federation (Development of tissue-engineered structures for cardiovascular surgery; N 121032300337-5).
Competing interests. The authors declare no conflict of interest.
Authors’ contribution. All authors made a substantial contribution to the conception of the work, acquisition, analysis, interpretation of data for the work, drafting and revising the work, final approval of the version to be published and agree to be accountable for all aspects of the work. T.A. Bergen, D.A. Sirota ― conception and design of the work; E. Kobelev, N.T. Pak, E.E. Kliver ― acquisition, analysis of data; E.E. Bobrikova, V.Yu. Usov ― interpretation of data; A.M. Chernyavskiy ― approved the final version of the work.
Consent for publication. Written consent was obtained from the patient for publication of relevant medical information and all of accompanying images within the manuscript in Digital Diagnostics journal.
Acknowledgments. We thank the Chief of the Institution of Experimental Biology and Medicine “E. Meshalkin National Medical Research Center” of the Ministry of Health of the Russian Federation MD Ph.D. professor Irina Yu. Zhuravleva for the opportunity to carry out this work.
作者简介
Evgenii Kobelev
E. Meshalkin National Medical Research Center
Email: kobelev_e@meshalkin.ru
ORCID iD: 0000-0002-5901-2271
SPIN 代码: 7828-9713
俄罗斯联邦, Novosibirsk
Natalya T. Pak
E. Meshalkin National Medical Research Center
Email: n_pak@meshalkin.ru
ORCID iD: 0000-0002-7842-9881
SPIN 代码: 1896-8447
MD, Cand. Sci. (Med.)
俄罗斯联邦, NovosibirskEvgeniya E. Bobrikova
E. Meshalkin National Medical Research Center
Email: bobrikova_e@meshalkin.ru
ORCID iD: 0000-0001-5985-4076
SPIN 代码: 6315-9772
俄罗斯联邦, Novosibirsk
Wladimir Y. Ussov
Tomsk National Research Medical Center
Email: ussov1962@yandex.ru
ORCID iD: 0000-0001-7978-5514
SPIN 代码: 1299-2074
MD, Dr. Sci. (Med.), Professor
俄罗斯联邦, TomskEvgeniy E. Kliver
E. Meshalkin National Medical Research Center
Email: ee_kliver@meshalkin.ru
ORCID iD: 0000-0002-3915-3616
SPIN 代码: 1511-3814
MD, Dr. Sci. (Med.)
俄罗斯联邦, NovosibirskDmitriy A. Sirota
E. Meshalkin National Medical Research Center
Email: d_sirota@meshalkin.ru
ORCID iD: 0000-0002-9940-3541
SPIN 代码: 4706-7549
MD, Cand. Sci. (Med.)
俄罗斯联邦, NovosibirskAleksandr M. Chernyavskiy
E. Meshalkin National Medical Research Center
Email: a_cherniavsky@meshalkin.ru
ORCID iD: 0000-0001-9818-8678
SPIN 代码: 5286-6950
MD, Dr. Sci. (Med.), Professor, Corresponding member of the Russian Academy of Sciences
俄罗斯联邦, NovosibirskTatyanа A. Bergen
E. Meshalkin National Medical Research Center
编辑信件的主要联系方式.
Email: bergen_t@meshalkin.ru
ORCID iD: 0000-0003-1530-1327
SPIN 代码: 5467-7347
MD, Dr. Sci. (Med.)
俄罗斯联邦, Novosibirsk参考
- Erbel R, Aboyans V, Boileau C. et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The task force for the diagnosis and treatment of aortic diseases of the European society of cardiology (ESC). Eur Heart J. 2014;35(41):2873–926. doi: 10.1093/eurheartj/ehu281
- Hiratzka LF, Bakris GL, Beckman JA, et al. Guidelines for the diagnosis and management of patients with thoracic aortic disease. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. J Am Coll Cardiol. 2010;55(14):e27–e129.
- Galizia MS, Bolen MA, Flamm S. MRI of the thoracic aorta. Applied Radiology. 2015;44(8):22–26. doi: 10.37549/ar2207
- Saliba E, Sia Y. The ascending aortic aneurysm: When to intervene? IJC Heart Vasculature. 2015;6:91–100. doi: 10.1016/j.ijcha.2015.01.009
补充文件