Creation of a training and test dataset with the disposition and transposition of overlaying electrocardiographic electrodes when recording electrocardiograms-12
- Authors: Gazashvili T.M.1, Drozdov D.V.2, Shutov D.V.3, Shkoda A.S.1
-
Affiliations:
- City Clinical Hospital No. 67 named after L.A. Vorokhobov
- National Medical Research Centre of Cardiology Named After Academician E.I. Chazov
- Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies
- Issue: Vol 4, No 2 (2023)
- Pages: 133-141
- Section: Datasets
- Submitted: 04.04.2023
- Accepted: 15.05.2023
- Published: 12.07.2023
- URL: https://jdigitaldiagnostics.com/DD/article/view/201870
- DOI: https://doi.org/10.17816/DD201870
- ID: 201870
Cite item
Abstract
BACKGROUND: Electrocardiography is one of the simplest, most widely used, inexpensive, and informative methods in functional diagnostics; yet, if performed poorly, its diagnostic value is sharply reduced. Several attempts were made to systematize errors and deviations in electrode application, but all concerned the most common options (rearrangement of red and yellow electrodes, yellow and green electrodes, and chest electrodes — above or below the standard scheme).
AIM: To create an electrocardiogram dataset with different options for transpositions and dispositions of electrodes during electrocardiogram recording.
MATERIALS AND METHODS: The study included patients aged 18–75 years (27 males and 22 females). All patients provided informed consent for electrocardiogram registration. During one visit, the cardiogram was recorded on the device “Modular system for recording and remote transmission of electrocardiograms (EASY ECG)” for each patient.
RESULTS: In all, 488 electrocardiograms were recorded in 49 patients. The results obtained indicate a significant variability of the electrocardiogram pattern. Visual analysis of the electrocardiograms revealed no difficulties in determining the transposition associated with rearranging the leads on the arms (RY) in the thoracic C1–C2. The placement of thoracic electrodes in contact cheek-to-cheek dispositions with the transfer of thoracic leads above or below two intercostals was reliably determined compared with the Wilson scheme. The transpositions of the yellow and green limb electrodes and the change in the position of the thoracic ones when they are “lined up” in a straight line, “bullied” between the ribs (curved), and confused in places C5 and C6 are difficult to determine even when comparing two cardiograms next to each other, with the correct and transpositional superposition of the electrodes. The initial changes on the electrocardiograms, physique type, breast size, or the presence of an implant most likely determine it.
CONCLUSION: An electrocardiography dataset was obtained using various electrode dislocation variants. The dataset consists of a series of electrocardiograms obtained for each patient with several electrode placement options and contains both normal and pathological electrocardiograms.
Full Text
BACKGROUND
Electrocardiography (ECG) is one of the simplest, most widespread, inexpensive, and informative techniques in cardiology; however, its diagnostic value is dramatically reduced if it is not performed correctly. The most common change in the recording technique is electrode displacement (dislocation). A disposition (a deliberate and necessary change in electrode placement) should be distinguished from a transposition (an erroneous change in electrode placement compared with the standard overlay pattern).
Several studies have attempted to systematize errors and deviations in electrode placement; however, all of them concerned the most frequent variants, such as relocation of red and yellow, yellow and green, and precordial electrodes above or below the standard pattern. [1-7] To avoid errors in the interpretation of ECG recordings, algorithms capable of detecting such errors are developed. Machine algorithms stably recognize right–left (RL) transposition.
To assess the quality and determine the criteria for the possibility of using such algorithms, ECG datasets should be created for training and testing both algorithms for automatic ECG analysis and by healthcare specialists, i.e., doctors and nursing staff.
This study aimed to create an ECG dataset with different electrode transpositions and dispositions during ECG recording for training and testing machine-learning systems.
MATERIALS AND METHODS
Inclusion criteria
Patients aged 18–75 years (27 men and 22 women) were included in the study. All patients gave voluntary informed consent for ECG recording.
Settings
The study was performed in the Moscow State Budgetary Institution City Clinical Hospital No. 67 named after L.A. Vorokhobov of Moscow Healthcare Department.
Description of treatment
The patients were divided into the following six arms:
1) Patients with normal ECG (recordings starting with 101, 102, 103, 104, 105, 106, 107, 108, 109, and 110).
2) Patients with ECG signs of left ventricular hypertrophy or complete left bundle branch block (recordings starting with 201, 202, 203, 204, 205, 206, 207, 208, and 209).
3) Patients with ECG signs of right bundle branch block (recordings starting with 301, 302, 303, 304, 305, and 306).
4) Patients with recorded ST (−) depression (recordings starting with 401, 402, 403, 404, 405, 406, 407, 408, and 409).
5) Patients with recorded ST(+) elevation, including the phenomenon of early ventricular repolarization (recordings starting with 501, 502, 503, 504, 505, 506, and 507).
6) Patients with any nonsinus rhythm that are preferably characterized by negative P waves in I, II, V1, and V2 leads (recordings starting with 601, 602, 603, 604, 605, 606, 607, and 608).
Cardiograms were recorded using EASY ECG Modular System for Recording and Remote Transmitting of ECGs according to TU 9441-001-42447560-2012 with Accessories (ATES MEDICA SOFT LTD, Russia, Registration Certificate No. RZN 2018/7062).
For ECG recording, operating silver/silver chloride electrodes were used with 26 × 47-mm plates (for limb ones) and 22-mm cups (for precordial ones).
Digitized cardiac signals were recorded in the European data format. [8] Recordings were made in 12 common leads with a sample rate of 500 Hz, the recording lasted for 10 s, and the signal magnitude was 10 mV. No signal filtering was performed, and the bandwidth was from 0.05 to 150 Hz.
Ethical review
The study was approved by the independent ethical committee of the Moscow Regional Branch of the Russian Society of Roentgenologists and Radiologists (RSRR MRB IEC).
RESULTS
Each patient underwent sequential ECG recording during one visit with correct electrode placement and different variants of dis- and transpositions. The coding and description of overlay patterns are provided in Table 1.
Table 1. Electrode placement variants and their coding
Russian wording | English equivalent | Part of the ECG filename | Comment | Incorrectly displayed leads |
Стандартное расположение электродов | Standard electrodes’ arrangement | dis_st | Correctly applied electrodes | All leads are correct |
Грудные электроды: на 2 межреберья выше стандартной схемы | Precordial electrodes’ misplacement: up to 2 intercostal spaces above the standard arrangement | dis_u2 | Occasionally required for clinical indications, but in general, it is the most common electrode misplacement | Correct: I, II, III, aVR, aVL, and aVF. Dislocated: V1, V2, V3, V4, V5, and V6 |
Грудные электроды: на 2 межреберья ниже стандартной схемы | Precordial electrodes’ misplacement: below to 2 intercostal spaces down the standard arrangement | dis_d2 | Occasionally required for clinical indications, but in general, it is electrode misplacement | Correct: I, II, III, aVR, aVL, and aVF. Dislocated: V1, V2, V3, V4, V5, and V6 |
Перепутаны красный (R) и жёлтый (L) электроды | Reversal of the two arm electrodes | trns_ry | Misplacement | Incorrect: I, II, III, aVR, aVL, and aVF. Correct: V1, V2, V3, V4, V5, and V6 |
Перепутаны жёлтый (L) и зелёный (F) электроды | Reversal of the left arm and left leg electrodes | trns_yg | Misplacement | Incorrect: I, II, III, aVR, aVL, and aVF. Correct: V1, V2, V3, V4, V5, and V6 |
Все грудные электроды расположены на прямой линии от C1–C6 | All chest electrodes are placed at the same line | trns_ln | Misplacement | Correct: I, II, III, aVR, aVL, aVF, and V1. Incorrect: V2, V3, V4, V5, and V6 |
Перепутаны C1–C2 | Reversal of the C1 and C2 electrodes | trns_12c | Misplacement | Correct: I, II, III, aVR, aVL, aVF, V3, V4, V5, and V6. Incorrect: V1 and V2 |
Перепутаны C5–C6 | Reversal of the C5 and C6 electrodes | trns-56c | Misplacement | Correct: I, II, III, aVR, aVL, aVF, V1, V2, V3, and V4. Incorrect: V5 and V6 |
Электроды C4, C5, C6 расположены очень близко друг к другу (соприкасаются) | The C4, C5, C6 electrodes are placed too close to each other (cheek to cheek) | trns_cls | Misplacement | Correct: I, II, III, aVR, aVL, aVF, V1, V2, and V3. Incorrect: V4, V5, and V6 |
Электроды C4, C5, C6 расположены по межреберью (не по горизонтальной линии, а искривляются вверх) | The C4, C5, C6 electrodes are misplaced along the intercostal space (not at a horizontal line, but curved upwards) | trns_crv | Misplacement | Correct: I, II, III, aVR, aVL, aVF, V1, V2, and V3. Incorrect: V4, V5, and V6 |
In total, 486 ECGs were recorded in 49 patients. The structure of the recorded ECGs is shown in Table 2.
Table 2. Allocation of cardiograms recorded in patients
Placement type Subgroup of ECG changes | Standard ECG placement | Dislocation of precordial electrodes | Transposition of limb electrodes | Transposition of precordial electrodes | Total |
Normal ECG | 10 | 20 | 20 | 49 | 99 |
ECG with LVH and CLBBB | 9 | 18 | 18 | 45 | 90 |
ECG with RBBB | 6 | 12 | 12 | 30 | 60 |
ECG with ST(−) depression | 9 | 18 | 18 | 43 | 88 |
ECG with ST(+) elevation | 7 | 14 | 14 | 35 | 70 |
ECG with any nonsinus rhythm | 8 | 15 | 16 | 40 | 79 |
Total | 49 | 97 | 98 | 242 | 486 |
Notes. ECG, electrocardiogram; CLBBB, complete left bundle branch block; LVH, left ventricular hypertrophy; RBBB, right bundle branch block.
After recording, all results were anonymized and pseudonymized1, placed, and annotated on the ECG.RU platform using a unified thesaurus. [9] Each ECG file was named according to the following principles: the first three digits referred to the patient subgroup number and serial number, and subsequent letters referred to the coding of electrode placement.
For example, the file name “101_dis_st” meant that this ECG was recorded in a patient with an unchanged ECG, and the electrodes were placed correctly. The file name “203_trns_crv” contains the ECG of a patient with left ventricular hypertrophy, and the C4, C5, and C6 electrodes are placed along the intercostal line (not along the horizontal line, but curved upward). The file name “602_trns_yg” contains the ECG of a patient with nonsinus rhythm, and the yellow and green electrodes are reversed. Examples of recorded ECGs are shown in pairs in Figures 1–3 (overlay pattern and corresponding ECG).
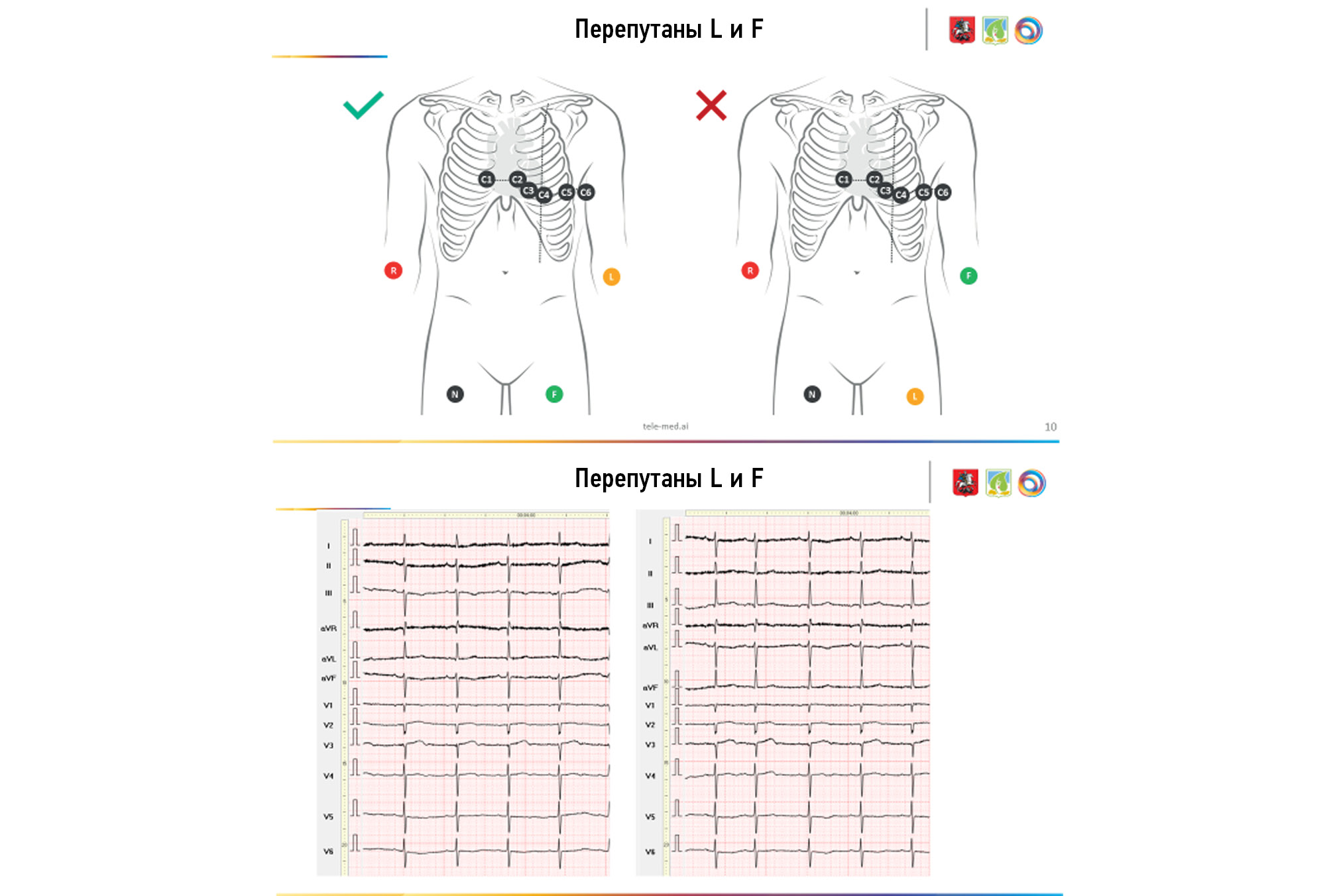
Fig. 1. Misplacement of L and F electrodes.
Fig. 2. Misplacement of C4–C6 electrodes.
Fig. 3. Dislocation of C4–C6 electrodes.
DISCUSSION
The obtained results indicate a significant variability of ECG patterns depending on the initial changes and, probably, the patient’s body type and state of mammary glands. Despite sufficient studies on the variability of normal ECG changes, [6–8] the variability of changes in the initial abnormal ECG is yet to be examined, which we will do in our next paper.
In the visual evaluation of the recorded ECGs, transposition was determined based on the relocation of the arm leads (red and yellow—RL) and precordial C1–C2 was not complicated. The placement of precordial cheek-to-cheek electrodes, in disposition with the transfer of the precordial leads higher or lower by two intercostal spaces than the Wilson scheme (upper2 and lower2), was less often reliably determined. Transpositions of yellow and green limb electrodes (LF), changes in the position of precordial electrodes, when they are in line, curved, or C5–C6 electrodes are reversed, are difficult to determine even when directly comparing two cardiograms, with correct placement and transposition of electrodes. This probably depends on baseline ECG changes, body type (normosthenic, hypersthenic, or asthenic), breast size, or presence of an implant. Certainly, issues such as the consideration of the built, presence of a transplant, possible detailing of the initial ECG changes according to the reduced thesaurus, and comparison of the efficiency of recognition by a specialist and automatic analysis algorithms, require further evaluations.
Despite the known disadvantages, considering the high importance of the issue and difficulty of obtaining qualitatively recorded data and annotated ECGs, the obtained set of ECGs was published under an open license and used for both verification of algorithms of automatic ECG analysis and training of doctors and nursing staff.
Study limitations
On patient examination, their height, weight, and built (somatotypes) were not always considered. Taking these factors into account will probably increase the accuracy of determining the type of electrode dislocation.
CONCLUSION
In this study, an ECG dataset with different electrode dislocation variants was obtained. The dataset consists of ECG series recorded in each patient with different electrode overlap variants. The set includes not only normal ECGs but also different variants of abnormal ECGs.
ADDITIONAL INFORMATION
Funding source. This article was not supported by any external sources of funding.
Competing interests. The authors declare that they have no competing interests.
Authors’ contribution. All authors made a substantial contribution to the conception of the work, acquisition, analysis, interpretation of data for the work, drafting and revising the work, final approval of the version to be published and agree to be accountable for all aspects of the work. D.V. Drozdov ― concept development, organization of annotation process, thesaurus development, author supervision; T.M. Gazashvili ― organization of ECG registration, depersonalization and transfer of records; D.V. Shutov ― concept development, organization of depersonalization, transfer, annotation, author supervision; A.S. Skoda ― general management, organization of the work of the center for instrumental diagnostics.
Acknowledgments. The authors express their gratitude to Medical Computer Systems LLC, personally to the director of the company Prilutsky Dmitry Anatolyevich and all employees of the platform ECG.ru. Meshcherina Tatiana Evgenievna and Shalmonova Elena Gennadievna for highly qualified ECG registration.
1 GOST R 55036-2012/ISO/TS 25237:2008. P85 Group. National Standard of the Russian Federation. Health Informatics. Pseudonymization. Access: https://docs.cntd.ru/document/1200100339.
About the authors
Tamara M. Gazashvili
City Clinical Hospital No. 67 named after L.A. Vorokhobov
Email: Tamaradoc24@gmail.com
ORCID iD: 0000-0002-5875-9699
SPIN-code: 4208-2303
Russian Federation, Moscow
Dmitry V. Drozdov
National Medical Research Centre of Cardiology Named After Academician E.I. Chazov
Email: cardioexp@gmail.com
ORCID iD: 0000-0001-7374-3604
SPIN-code: 2279-9657
MD, Cand. Sci. (Med)
Russian Federation, MoscowDmitry V. Shutov
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies
Email: ShutovDV@zdrav.mos.ru
ORCID iD: 0000-0003-1836-3689
SPIN-code: 9381-2456
MD, Dr. Sci. (Med)
Russian Federation, MoscowAndrey S. Shkoda
City Clinical Hospital No. 67 named after L.A. Vorokhobov
Author for correspondence.
Email: a.shkoda@67gkb.ru
ORCID iD: 0000-0002-9783-1796
SPIN-code: 4520-2141
MD, Dr. Sci. (Med)
Russian Federation, MoscowReferences
- Rosen AV, Koppikar S, Shaw C, Baranchuk A. Common ECG lead placement errors. Part I: Limb lead reversals. Int J Med Students. 2014;2(3):92–98. doi: 10.5195/ijms.2014.95
- Rosen AV, Koppikar S, Shaw C, Baranchuk A. Common ECG lead placement errors. Part II: precordial misplacements. Int J Med Students. 2014;2(3):99–103. doi: 10.5195/ijms.2014.96
- Jekova I, Krasteva V, Leberet R, et al. Inter-lead correlation analysis for automated detection of cable reversals in 12/16-lead ECG. Comput Methods Programs Biomed. 2016;(134):31–41. doi: 10.1016/j.cmpb.2016.06.003
- Kania M, Rix H, Fereniec M, et al. The effect of precordial lead displacement on ECG morphology. Med Biological Engineering Computing. 2014;52(2):109–119. doi: 10.1007/s11517-013-1115-9.
- Wenger W, Kligfield P. Variability of precordial electrode placement during routine electrocardiography. J Electrocardiol. 1996;29(3):179–184. doi: 10.1016/s0022-0736(96)80080-x
- García-Niebla J, Llontop-García P, Valle-Racero JI, et al. Technical mistakes during the acquisition of the electrocardiogram. Ann Noninvasive Electrocardiol. 2009;14(4):389–403. doi: 10.1111/j.1542-474X.2009.00328.x
- Peberdy MA, Ornato JP. Recognition of electrocardiographic lead misplacements. Am J Emergency Med. 1993;11(4):403–405. doi: 10.1016/0735-6757(93)90177-d
- Kemp B, Olivan J. European data format ‘plus’ (EDF+), an EDF alike standard format for the exchange of physiological data. Clin Neurophysiol. 2003;114(9):1755–1761. doi: 10.1016/s1388-2457(03)00123-8
- Drozdov DV, Shutov DV, Gazashvili TM, et al. Coordination of medical ECG descriptions using a thesaurus (list of standard phrases) of conclusions. Medical Alphabet. 2022;(10):19–26. (In Russ). doi: 10.33667/2078-5631-2022-11-19-26
Supplementary files