Using a mobile computer tomography scanner in a field hospital setting to manage patients with COVID-19
- Authors: Kudryavtsev N.D.1, Petraikin A.V.1, Ahkmad E.S.1, Kiselev F.A.1, Burashov V.V.1, Mukhortova A.N.1, Soldatov I.V.1, Shkoda A.S.2
-
Affiliations:
- Moscow Center for Diagnostics and Telemedicine
- City Clinical Hospital No. 67 named after L.A. Vorokhobov
- Issue: Vol 4, No 3 (2023)
- Pages: 427-438
- Section: Correspondence
- Submitted: 11.04.2023
- Accepted: 17.04.2023
- Published: 26.09.2023
- URL: https://jdigitaldiagnostics.com/DD/article/view/321670
- DOI: https://doi.org/10.17816/DD321670
- ID: 321670
Cite item
Abstract
The global outbreak of COVID-19 has posed unprecedented challenges to healthcare systems worldwide. Healthcare administrators had to make quick and effective decisions to ensure high quality of medical care standards in new conditions. The need to form a reserve bed fund during the pandemic was due to the high load on city hospitals in Moscow. Due to this fact, temporary reserved hospitals for COVID-19 patients were organized in non-core facilities, such as ice arenas, shopping malls, and exhibition pavilions. This urgency prompted a search for solutions that could provide the necessary level of diagnosis and treatment appropriate to specialized medical facility. Given the technical and time constraints associated with the installation of a fixed computer tomographic scanner, the deployment of mobile computer tomographic scanners emerged as a viable option.
The study aims to share insights gained from using a mobile computer tomographic scanner within a temporary backup hospital setting to treating patients with COVID-19 coronavirus infection. The paper discusses the features, advantages, and disadvantages of mobile computer tomography. It also presents hardware and control room layouts, along with the placement options for the computer tomography device. The research includes the results of dosimetry studies and provides a clinical assessment of the applicability of this type of diagnostic devices.
Full Text
INTRODUCTION
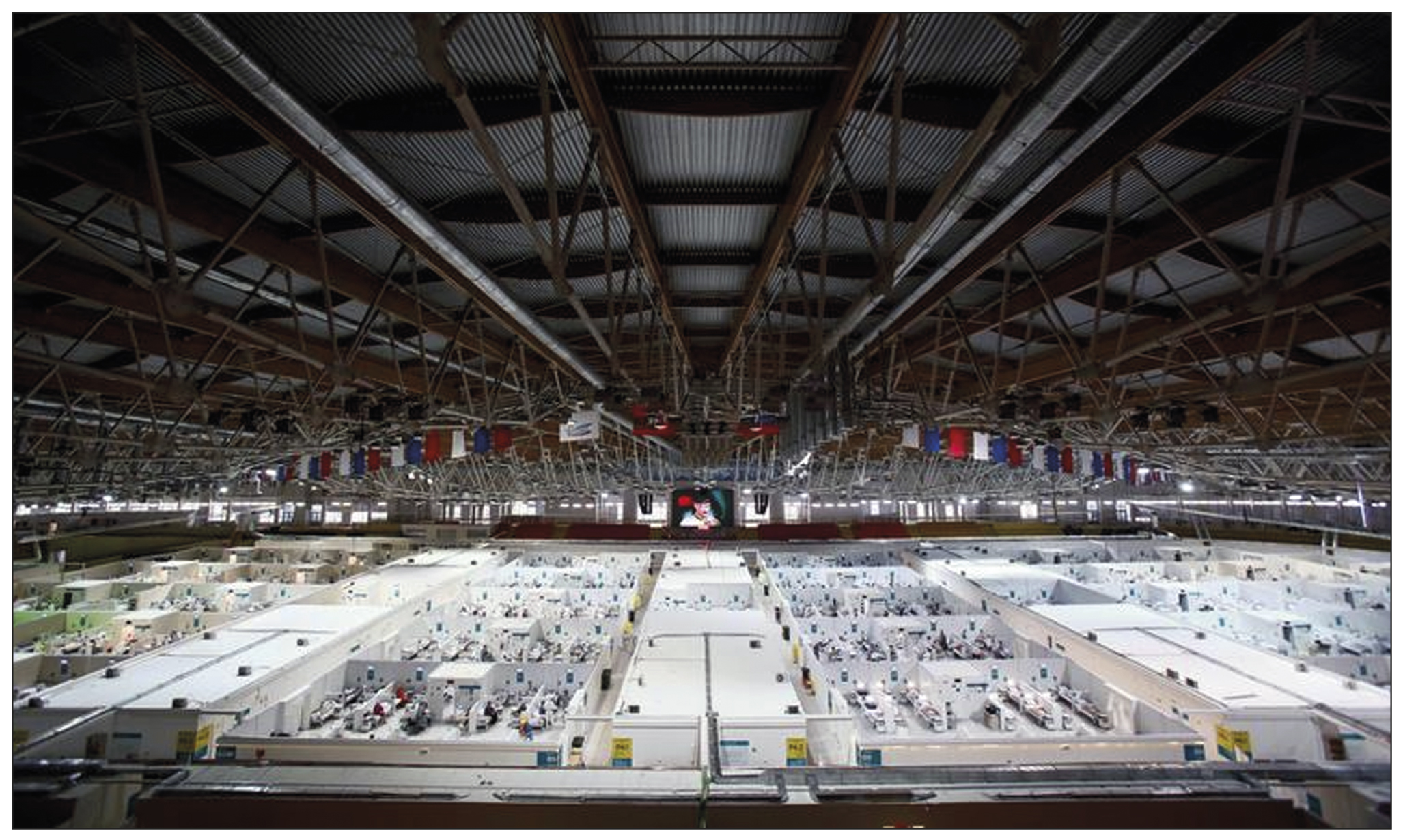
During the COVID-19 pandemic, in Moscow, a reserve bed capacity was required due to the high load on city hospitals. Field COVID-19 hospitals were deployed in noncore buildings (ice arenas, shopping centers, and exhibition halls), and special solutions were required to provide the necessary level of diagnosis and treatment comparable with a specialist healthcare institution [1]. One field hospital was located at the Krylatskoye Ice Palace (State Budgetary Healthcare Institution “L.A. Vorokhobov City Clinical Hospital No. 67,” Department of Healthcare of Moscow Fig. 1).
Fig. 1. A field hospital for COVID-19 patients in Krylatskoye Ice Palace (Moscow, Russia). Reuters (https://pictures.reuters.com/).
Diagnostic radiology techniques (particularly computed tomography [CT]) are recommended for detecting signs of COVID-19 pneumonia and to establishing a differential diagnosis for other lung diseases and assessing disease severity, changes in a patient’s condition, and treatment effectiveness [2–4]. A mobile Airo TruCT tomograph (Stryker, USA) was deployed due to technical and time constraints of employing a stationary computed tomograph.
The purpose of this study was to assess the efficacy of mobile CT in a field hospital for COVID-19 patients.
A MOBILE COMPUTED TOMOGRAPHER: EFFECTIVENESS IN SETTING OF A FIELD HOSPITAL FOR COVID-19 PATIENTS
General characteristics of a mobile CT
The Airo TruCT is designed for use in neurosurgery operating rooms, but the manufacturer claims that it can also be used to diagnose urgent conditions in other anatomical areas.1 Airo TruCT has a compact size (Fig. 2), making it simple to install and transport. A moveable base, a gantry with a 107-cm aperture, and 32 rows of 1-mm detectors comprise this CT system. CT is controlled by a hard-wired console connected by a 5-m wire (Fig. 3). The mobile CT is adaptable to a variety of power supply conditions and is linked to a 1.5-kW network. A power supply system, on the other hand, permits scanning at 120 kV and 250 mA, which corresponds to a power of 30 kW.
Fig. 2. A mobile computed tomograph ready for scanning.
Fig. 3. Airo TruCT control console.
Location and dosimetry
In accordance with current rules and measurement methods, a CT room was certified for compliance with technical requirements during technical equipment testing (monitoring of operating parameters) and radiation monitoring at the workplace and adjacent rooms.
The CT room is located on the first floor of Krylatskoye Ice Palace, in the Emergency Department (Fig. 4). Due to the increased patient flow and off label use of this device, some technical solutions were required:
- The CT console was relocated to the control room to ensure technicians’ radiation safety.
- A video system was constructed to monitor the patient’s status and the progress of the scanning because there was no viewing in the control room.
- Baofeng portable radios were used for communicating with patients during scanning due to the lack of built-in voice commands for holding breath.
Radiation protection in adjacent rooms complied with Russian requirements for design and operation of X-ray rooms, considering operating parameters of Airo TruCT (during scanning, the gantry moves, whereas the patient table is fixed). Sheets of X-ray protective plasterboard from Knauf (Iphofen, Germany) were used to safeguard stationary building envelops.
Dosimetry monitoring at workplaces, in adjacent rooms, and in adjacent regions revealed that exposure levels did not exceed values defined in current regulatory regulations at the observed spots (see Fig. 4).
Fig. 4. The project of a computed tomography room, control room, and radiologist’s office: Zone A—pavilion; Zone B—technical area; Zone C—hallway (zones A to C are areas without permanent presence of personnel).
Technical quality control
In accordance with current norms, a standard assessment of the CT system’s operational parameters was performed2. Sum filtering, half-value layer, anode voltage ripple, anode voltage, exposure time, radiation dose linearity, radiation dose repeatability, and image quality characteristics were evaluated.
According to the test results, the CT system meets performance and standard requirements.
Clinical use
A field hospital accepted patients with mild and moderate COVID-19 [2] with CT-1 and CT-2 lung parenchyma damage, requiring hospital treatment and observation. The chest CT was performed on all hospitalized patients. The only exception was for patients who had a recent CT (4 days). CT data revealed that 155 (31.0%) of 500 randomly selected patients had CT-1, 202 (40.4%) had CT-2, 109 (21.8%) had CT-3, and 34 (6.8%) had CT-4. Due to the high-power consumption and possibility of X-ray tube overheating during multiphase scanning, contrast-enhanced CT was not performed. The relative duration of scanning was a limitation of that technique.
Computed tomography scans of the brain and head, abdomen and retroperitoneum, pelvic organs, spine, and extremities were conducted when clinically required (scanning parameters are listed in Table 1).
Table 1. Standardized scanning protocols for different anatomical regions
Anatomic region parameter | Chest | Brain | Abdomen |
Scanning direction | Craniocaudal | Craniocaudal | Craniocaudal |
Scan type | Spiral | Spiral | Spiral |
Electric voltage (kV) | 120 | 120 | 120 |
Electric current (mA) | 38 | 155 | 69 |
Slice thickness (mm) | 1.0 | 1.0 | 1.0 |
Pitch factor | 1.415 | 1.415 | 1.415 |
X-ray tube rotation time (s) | 1.92 | 1.92 | 1.92 |
Reconstruction matrix (px) | 512 × 512 | 512 × 512 | 512 × 512 |
Duration of scan (s) | 12 | 8 | 16 |
Absorbed radiation dose (mGy*cm) | 230.7 | 1,186.8 | 564 |
Scan length (cm) | 30 | 20 | 40 |
The system’s wide (107 cm) gantry aperture was an apparent advantage.
Chest CT was conducted in the majority of cases to obtain a diagnosis or to provide continuing observation for patients with COVID-19 pneumonia. The scanning parameters (Table 1) enable us to obtain images of adequate quality to differentiate between viral pneumonia, cardiogenic pulmonary edema, and bacterial pneumonia. Fig. 5 shows CT data for COVID-19-associated viral pneumonia patients.
Fig. 5. Axial computed tomographic slices of chest organs in the lung window: (a) polymorphic, predominantly subpleural areas of ground-glass opacity, corresponding to the CT image of viral pneumonia (including COVID-19), CT-1, and (b) multiple polymorphic areas of parenchyma compaction with a tendency to merge, with ground-glass opacity areas and mild reticular changes, CT-3.
Long-term (15–25 s) scanning was too long for patients with respiratory insufficiency to remain their breath for the entire examination compared with stationary CT (3–5 s). As a result, motion artifacts (Fig. 6a) and steps (Fig. 6b) were present in CT images produced by breathing motions of the chest (Fig. 6).
Fig. 6. Axial and sagittal computed tomographic slices of chest organs in the lung window: (a) motion artifacts and (b) step artifacts caused by respiratory chest movements during scanning.
Brain CT was used to diagnose acute cerebrovascular accident, intracranial hematomas, brain tumors, and traumatic skull injuries (Fig. 7).
Fig. 7. Axial computed tomographic images of the brain: (a) reconstruction of a 3-mm low-density area at the anterior horn of the left lateral ventricle, in the periventricular, subcortical direction (CT image of subacute cerebrovascular accident of the left middle cerebral artery), and (b) a 1-mm site of subarachnoid hemorrhage with blood breakthrough into the ventricular system (vicarious hydrocephalus).
Windmill artifacts (Fig. 8a) were mixed with strike artifacts and helical scanning [5], and artifacts intensified at the level of skull base, where significant beam hardening and scattering artifacts occurred (Fig. 8, b). Therefore, subtentorial brain areas were challenging to assess.
Fig. 8. Axial (a) and sagittal (b) computed tomographic images of the head in the region of the posterior cranial fossa and base of skull showed windmill, strike, beam hardening, and scattering artifacts. Area of bone structures and the posterior fossa is hard to evaluate.
Abdomen CT was used to assess acute abdominal problems, such as suspected intestinal blockage, and detect free liquid or gas (Fig. 9).
Fig. 9. Axial computed tomographic images of the abdomen: (a) CT image of multiple hypodense lesions of both liver lobes, helical artifacts, and gas interface artifacts in the intestinal area and (b) CT image of a strangulated umbilical hernia.
Artifacts were also identified during abdomen CT at the point of contact of various density media, such as intestine gas and surrounding soft tissue (gas-interface artifact) and helical scanning artifacts.
The scanning parameters (Table 1) enable the acquisition of images of sufficient quality for the diagnosis of abdominal and retroperitoneal disorders (liver steatosis, gallstone disease, adrenal hyperplasia and incidentaloma, kidney cysts and urolithiasis, focal liver lesions, and other conditions).
Evaluation of a mobile CT effectiveness
From the start of the field hospital operation (August 11, 2020) to January 31, 2021, 6,264 CT scans were performed, including 6,126 (97.80%) chest CTs, 98 (1.56%) brain CTs, 31 (0.49%) abdomen CTs, and nine (0.14%) other CTs. The average radiation exposure was 3.22 mSv for chest CT, 2.49 mSv for brain CT, and 8.46 mSv for abdomen CT.
To assess CT effectiveness, a load equal to the ratio of the average number of CT scans per day to the Moscow standard (41 scans per day for three-shift work) was determined. The average number of scans performed in such case was 44 a day (ranging 14 scans at the start of the temporary hospital operation to >110 scans per day in days with the highest inpatient flow). This amounted to 106% of the recommended load. When Airo TruCT was compared with stationary Aquilion Prime or Revolution EVO tomographs, the utilization levels were equivalent. The average level of utilization for stationary CT in two hospitals was 113%, according to data. As previously stated, no contrast-enhanced CT scans were conducted.
Such a load validated excellent efficacy of using a mobile CT in temporary hospitals. However, technical difficulties were recorded during periods of extensive mobile CT use, which could result in the tomograph being shut down for maintenance. The manufacturer suggests conducting six scans per hour to extend the operational time of a mobile CT and avoid technical concerns.
DISCUSSION
The COVID-19 pandemic has raised various challenges regarding inpatient care organization, such as how to enhance bed capacity, organize field hospitals, and provide logistics for such solutions [6].
One method for ensuring CT availability in field hospitals is to use tiny transportable computed tomographs. This paper summarizes experience of using an Airo TruCT mobile CT. Apparent advantages of this CT system include compatibility with various power supply parameters, ease of installation and transportation, and the ability to quickly design a room for a mobile CT scan and put this equipment into operation.
A mobile CT generated acceptable quality chest CT images detecting viral pneumonia (see Fig. 5 a), and the patient capacity was sufficient for a temporary hospital with 1,300 beds in overload circumstances. The peak load was 110 scans per day, with an average of 44. This system differs from modular and mobile CTs mounted on trailers [7], mostly due to the use different types of CT.
However, some limitations were observed, indicating that the present modification’s usage of a mobile CT was a forced solution. Some motion artifacts developed as a result of low scanning speed compared with stationary CT scanners. The caudal–cranial direction was proposed for chest CT scanning to limit the amount of respiratory artifacts [8]. Due to the configuration of the CT room (gantry movement was limited due to insufficient console wire length) in our situation of using Airo TruCT, such a solution proved unacceptable. The problem was fixed by postponing the command to hold the breath for 3–4 s after the scan began. Although the apical lung segment exhibited significant motion abnormalities and steps, the basal portions were clearly visible. This observation is significant because patches of ground-glass opacity or consolidation are precisely situated in the dorsal sections of the lower lobes in COVID-19 pneumonia [9]. Simple technical solutions, such as handheld transceivers and video communication, were also used to adopt off-label use of Airo TruCT. Due to the significant number of artifacts detected, additional scanning, reconstruction, and postprocessing algorithms should be developed, and scanning parameters should be optimized [10].
Despite the mobility and easy installation of mobile CTs, design of an equipment room should comply with all radiation safety requirements (see Fig. 2).
In addition to field COVID-19 hospitals, mobile CTs can be used efficiently in healthcare institutions where there are no conditions for fixed CT installation or when the main CT scanner has failed. Mobile CT scanners can be used in remote communities and temporary mobile hospitals for emergency recovery.
The use of mobile CT also opens up new avenues for scientific research; for example, in our case, the mobile CT was used to investigate the influence of COVID-19 on the cardiovascular system [11]. When preforming chest, brain, abdomen, and retroperitoneum CT at temporary hospital for COVID-19 patients, the use of Airo TruCT provide requisite diagnostic effectiveness.
Based on the identified disadvantages, a list of requirements for mobile CT systems was prepared, and the need to develop a new type of CT was demonstrated, including high compatibility with various power supply sources, the ability to quickly design rooms for CT deployment in temporary hospitals, and the ability of use in emergency situations and remote areas with unprepared infrastructure.
CONCLUSION
The installation of mobile CT in a field COVID-19 hospital was a forced solution due to the rapid development of the pandemic. The Airo TruCT is intended for use in neurosurgical operating rooms. Despite the off-label use, the mobile CT produced images of satisfactory quality. A fixed CT situated on a trailer or a separate module is an alternative to mobile CT, although this type of equipment has its disadvantages (e.g., difficult transport and placement outside the healthcare institution and problems with scanning in severe patients). In turn, the Airo TruCT has excellent mobility and reduced space and power requirements, allowing it to be transported by a single person. However, the high mobility of this tomograph affects the quality of images.
ADDITIONAL INFORMATION
Funding source. This article was prepared by a group of authors as a part of the research and development effort titled “Theoretical and methodological framework for digital transformation in radiology”, (USIS No. 123031400118-0) in accordance with the Order No. 1196 dated December 21, 2022 “On approval of state assignments funded by means of allocations from the budget of the city of Moscow to the state budgetary (autonomous) institutions subordinate to the Moscow Health Care Department, for 2023 and the planned period of 2024 and 2025” issued by the Moscow Health Care Department.
Competing interests. The authors declare that they have no competing interests.
Authors’ contribution. All authors made a substantial contribution to the conception of the work, acquisition, analysis, interpretation of data for the work, drafting and revising the work, final approval of the version to be published and agree to be accountable for all aspects of the work. N.D. Kudryavtsev ― the concept of publication, text writing, clinical analysis of mobile CT; A.V. Petraikin ― clinical analysis of mobile CT; E.S. Akhmad ― technical quality control of mobile CT, text writing; F.A. Kiselev, V.V. Burashov ― technical quality control of mobile CT; A.N. Mukhortova ― evaluation of the effectiveness of the use of mobile CT; I.V. Soldatov ― design of the radiology department, text editing; A.S. Shkoda ― organization of the work in the radiology department, text editing.
About the authors
Nikita D. Kudryavtsev
Moscow Center for Diagnostics and Telemedicine
Author for correspondence.
Email: n.kudryavtsev@npcmr.ru
ORCID iD: 0000-0003-4203-0630
SPIN-code: 1125-8637
Russian Federation, Moscow
Alexey V. Petraikin
Moscow Center for Diagnostics and Telemedicine
Email: PetryajkinAV@zdrav.mos.ru
ORCID iD: 0000-0003-1694-4682
SPIN-code: 6193-1656
MD, Dr. Sci. (Med.), Associate Professor
Ekaterina S. Ahkmad
Moscow Center for Diagnostics and Telemedicine
Email: e.ahkmad@npcmr.ru
ORCID iD: 0000-0002-8235-9361
SPIN-code: 5891-4384
Russian Federation, Moscow
Fyodor A. Kiselev
Moscow Center for Diagnostics and Telemedicine
Email: KiselevFA@zdrav.mos.ru
ORCID iD: 0009-0006-6472-8940
Russian Federation, Moscow
Vyacheslav V. Burashov
Moscow Center for Diagnostics and Telemedicine
Email: BurashovVV@zdrav.mos.ru
ORCID iD: 0000-0001-9250-0667
SPIN-code: 4308-0912
Russian Federation, Moscow
Anna N. Mukhortova
Moscow Center for Diagnostics and Telemedicine
Email: a.mukhortova@npcmr.ru
ORCID iD: 0000-0001-9814-3533
SPIN-code: 9051-1130
Russian Federation, Moscow
Iliya V. Soldatov
Moscow Center for Diagnostics and Telemedicine
Email: i.soldatov@npcmr.ru
ORCID iD: 0000-0002-4867-0746
SPIN-code: 4065-6048
Russian Federation, Moscow
Andrey S. Shkoda
City Clinical Hospital No. 67 named after L.A. Vorokhobov
Email: a.shkoda@67gkb.ru
ORCID iD: 0000-0002-9783-1796
SPIN-code: 4520-2141
MD, Dr. Sci. (Med), Professor
Russian Federation, MoscowReferences
- Morozov SP, Kuzmina ES, Ledikhova NV, et al. Mobilizing the academic and practical potential of diagnostic radiology during the COVID-19 pandemic in Moscow. Digital Diagnostics. 2020;1(1):5–12. (In Russ). doi: 10.17816/DD51043
- Prevention, diagnosis and treatment of new coronavirus infection (2019-nCoV): temporary guidelines. Version 17 (12/14/2022). (In Russ). Available from: https://static-0.minzdrav.gov.ru/system/attachments/attaches/000/061/254/original/%D0%92%D0%9C%D0%A0_COVID-19_V17.pdf?1671088207. Accessed: 15.03.2023. (
- De Smet K, De Smet D, Ryckaert T, et al. Diagnostic performance of chest CT for SARS-CoV-2 infection in individuals with or without COVID-19 symptoms. Radiology. 2021;298(1):E30–E37. doi: 10.1148/radiol.2020202708
- Huang Y, Cheng W, Zhao N, et al. CT screening for early diagnosis of SARS-CoV-2 infection. Lancet Inf Dis. 2020;20(9):1010–1011. doi: 10.1016/S1473-3099(20)30241-3
- Barrett JF, Keat N. Artifacts in CT: Recognition and avoidance. RadioGraphics. 2004;24(6):1679–1691. doi: 10.1148/rg.246045065
- Samorodskaja IV, Larina VN, Nazimkin KE, Larin VG. Organizational and clinical problems of outpatient COVID-19 diagnostics. Vrach. 2020;31(5):23–30. (In Russ). doi: 10.29296/25877305-2020-05-05
- Cester G, Giraudo C, Causin F, et al. Retrospective analysis of a modified organizational model to guarantee CT workflow during the COVID-19 outbreak in the Tertiary Hospital of Padova, Italy. J Clin Med. 2020;9(9):3042. doi: 10.3390/jcm9093042
- Bates DD, Vintonyak A, Mohabir R, et al. Use of a portable computed tomography scanner for chest imaging of COVID-19 patients in the urgent care at a tertiary cancer center. Emerg Radiol. 2020;27(6):597–600. doi: 10.1007/s10140-020-01801-5
- Khristenko EA, von Stackelberg O, Kautsor HU, et al. CT patterns in COVID-19 associated pneumonia: Standardization of research descriptions based on the Fleischner Society Glossary. Rejr. 2020;10(1):16–26. (In Russ). doi: 10.21569/2222-7415-2020-10-1-16-26
- Kyriakou Y, Meyer E, Prell D, Kachelriess M. Empirical beam hardening correction (EBHC) for CT. Med Phys. 2010;37(10):5179–5187. doi: 10.1118/1.3477088
- Aliev AF, Kudryavtsev ND, Petryaykin AV, et al. Changing of pulmonary artery diameter in accordance with severity of COVID-19 (assessment based on non-contrast computer tomography). Digital Diagnostics. 2021;2(3):249–260. (In Russ). doi: 10.17816/DD76726
Supplementary files