Testicular rupture in a young patient: diagnostic value of contrast-enhanced ultrasonography
- Авторлар: Eusebi L.1, Paparella M.T.2, Marconi A.3, Guglielmi G.2,4
-
Мекемелер:
- Radiology Unit, “Carlo Urbani” Hospital
- Department of Clinical and Experimental Medicine, Foggia University School of Medicine
- Department of Urology, “Carlo Urbani” Hospital
- Radiology Unit, Barletta University Campus UNIFG, “Dimiccoli” Hospital
- Шығарылым: Том 3, № 1 (2022)
- Беттер: 78-85
- Бөлім: Case reports
- ##submission.dateSubmitted##: 13.12.2021
- ##submission.dateAccepted##: 02.03.2022
- ##submission.datePublished##: 24.04.2022
- URL: https://jdigitaldiagnostics.com/DD/article/view/90277
- DOI: https://doi.org/10.17816/DD90277
- ID: 90277
Дәйексөз келтіру
Аннотация
Testicular rupture after a blunt scrotal trauma is characterized by tearing of the tunica albuginea that result in the extrusion of the seminiferous tubules.
Imaging, particularly ultrasonography, plays a crucial role in the assessment of scrotal trauma and directs patient management toward conservative or surgical treatment. Conventional B-mode and color Doppler ultrasonography are the main imaging techniques in the evaluation of the testicle in trauma but may underestimate the extent of injury. The most important information for the surgeon is the integrity or interruption of the tunica albuginea and the extent of vital testicular tissue. The latter is often difficult to assess with conventional ultrasonography because the injured testicle is often hypovascular even in vital regions due to testicular edema that compromises vascular flow. The selective use of advanced techniques such as contrast-enhanced ultrasonography is important in identifying testicular viability when color Doppler ultrasonography is equivocal.
This case report describes the evaluation and management of a blunt testicular trauma in a 15-year-old football player.
Толық мәтін
BACKGROUND
Scrotal trauma in young men accounts for less than 1% of all trauma-related injuries [1]. Testicular ruptures are seen in approximately 1.5% of cases of blunt scrotal trauma [2]. Less than 60 cases have been reported over the past decade [3]. The testicles are protected in their mobility within the scrotum by the tunica albuginea, laxity of the overlying skin, and contraction reflex of the cremasteric muscles. The tunica albuginea, with its great tensile strength, plays a crucial role in protecting the testicle; it can withstand a force of up to 50 kg without breaking [2]. The laxity of the genital skin can protect the underlying organs from blunt trauma allowing them to slip away from the point of contact; nevertheless, excessive skin laxity can lead to serious injury if the genital skin remains trapped in rotating machinery, causing avulsion and rupture of one or both testicles [4]. Sports activities account for more than 50% of all cases of testicular injuries, and motor vehicle collisions is another cause of scrotal trauma [5, 6]. Blunt injuries are noninvasive injuries due to the high energy transferred during contact with a solid object (e.g., from a kick in the groin or from the impact of a baseball or hockey bat). The main injury mechanism is the crushing of the testicle against the pubic symphysis or between the thighs. In most men, the right testicle is injured more frequently because it has an anatomical position slightly higher than that of the left testicle [7]. Scrotal trauma causes hemorrhage and infarction of the testicular parenchyma, which could lead to necrosis. In severe injuries, the disruption of the tunica albuginea accompanied by parenchymal protrusion can occur. It represents an indication for urgent surgery to salvage the testis [8]. Moreover, early repair is crucial, as rupture can damage the blood–testis barrier, with subsequent antibody formation against sperm cells leading to infertility [9]. This case study describes the evaluation and management of a blunt testicular trauma in a 15-year-old football player.
DESCRIPTION OF THE CASE
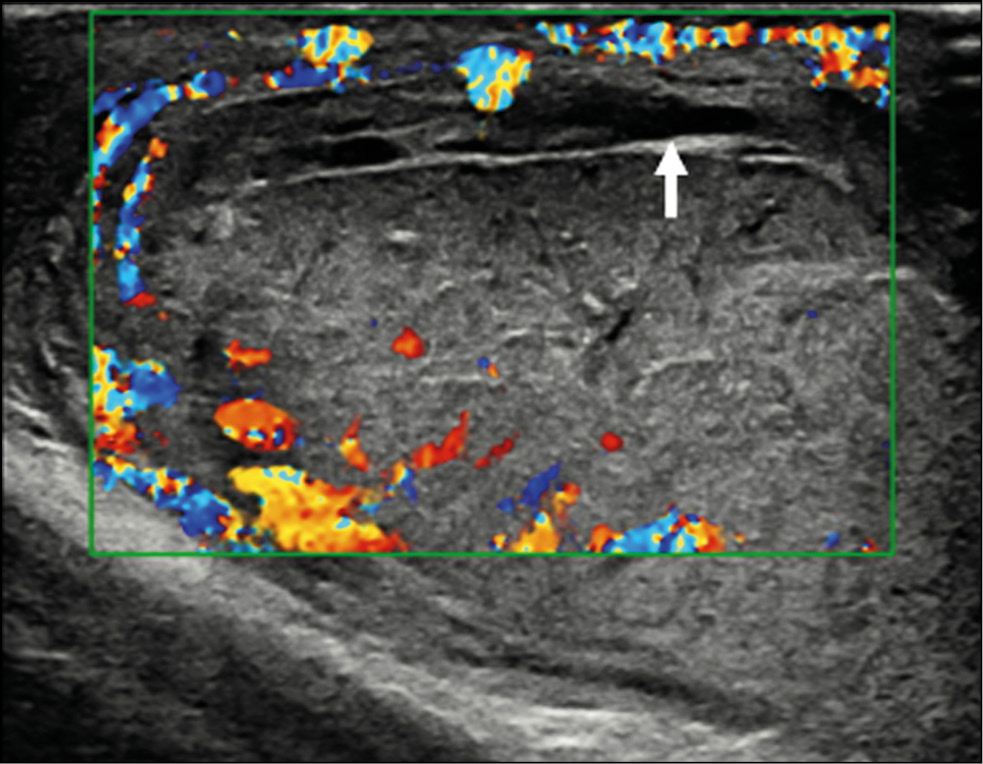
A healthy 15-year-old male teen was hit in the scrotum with a kick in the groin during a football match. He had an immediate and severe pain. After a few hours, although symptoms had improved, he presented to our emergency department with persistent swelling and purplish discoloration of the left scrotum. He did not report any other injuries. The genitourinary examination revealed that the left hemiscrotum was about two times larger than the right with severe ecchymosis. The left testicle was difficult to palpate because of pain and swelling, whereas the right testicle had a normal size and did not reveal any palpable abnormalities. The cremasteric reflex was not elicited on the left side. Scrotal ultrasonography (US) showed moderate scrotal edema and hematocele with a discontinuity in the tunica albuginea characterized by an abnormal contour (Figure 1). Color Doppler US (CDUS) documented a loss of vascularization in the upper pole that extruded into the broken portion of the testicle of approximately 2.5 cm (Figure 2) but no evidence of torsion or infarction. Urology consultation was requested, and a contrast-enhanced US (CEUS) was performed, which confirmed the diagnosis of testicular rupture and determined the amount of the vital parenchyma (Figure 3). The patient was hospitalized for urgent examination of the left hemiscotum based on the US results. During surgery, a large hematocele was evacuated, and a closer inspection of the testicle revealed a lesion of the tunica albuginea. Primary closure of the tunica was performed (Figure 4). The patient made an uneventful recovery, and he was discharged after 4 days.
Figure 1. B-mode ultrasonography images. (a) Interruption of the tunica albuginea with the protrusion of echogenic material (arrow) that represents an index of breaking. (b) Hematocele of moderate size (arrow) and a heterogeneous appearance of testicular parenchyma, attributable to an intratesticular contusion.
Figure 2. Color Doppler ultrasonography image showing an irregular testicular morphology with an avascular area at the breaking point (arrow).
Figure 3. Contrast-enhanced ultrasonography image determines the extent of vital parenchyma, helping in the preoperative decision-making process, and allows the recovery of vital testicular tissue, avoiding the need for orchidectomy.
Figure 4. Intraoperative images. (a) Confirmed rupture of the tunica albuginea. (b) Primary albuginea closure.
DISCUSSION
The differential diagnosis of scrotal lesions includes epididymitis, orchitis, incarcerated inguinal hernia, testicular infarction, testicular fracture or rupture, testicular torsion, appendicular torsion, dislocated testicles, hydrocele, or hematocele [10]. CDUS is the first-line imaging modality for studying traumatic pathology of the scrotum according to the guidelines of the European Association of Urology [11]. Thus, evaluating vascular perfusion and testicular integrity is important to distinguish testicular rupture from other lesions. Using modern ultrasonic equipment, sensitivity and specificity of 95%–100% are now possible for the diagnosis of testicular rupture [12]. The normal tunica albuginea appears as a thin hypoechoic line surrounding the testicular parenchyma. It can be difficult to appreciate it in the presence of hematocele. The regularity of the testicular contour should be checked in addition to the integrity of the tunica albuginea. Essentially, when testicular rupture occurs, the testicle loses its normal oval morphology because of parenchymal extrusion [13]. Thus, the irregularity of the testicle’s morphology is an indirect sign of ruptured tunica albuginea. Additional US findings include heterogeneous echotexture, rupture of the vaginal tunic, fracture lines through the testicle, decrease or loss of blood flow, scrotal thickening, and hematocele formation. CDUS is indispensable in the evaluation of a post-traumatic scrotum [14] since the rupture of the tunica albuginea is always associated with a rupture of the tunica vasculosa (composed of capsular arteries), resulting in a loss of the vascular signal of the underlying parenchyma. This aspect is extremely important because it can help determine the viability of the testicular parenchyma [15]. However, CDUS can be equivocal in acute cases because it may not detect low-flow states, particularly in pediatric patients [16], and is considered unreliable in defining ischemia [17] that could cause a delay in appropriate surgical treatment. CEUS can be proposed in cases where conventional US diagnosis remains inconclusive. CEUS is very sensitive to reveal the parenchymal vascularity and its changes in the damaged testicle [18]. The official guidelines of the European Federation of Societies for Ultrasound in Medicine and Biology describe the usefulness of CEUS in many areas [19]. Usually, 4.8 mL of SonoVue™ (Bracco Spa, Milan) is used. Contrast agents for CEUS examination are not nephrotoxic, the phospholipidic shell is metabolized by the liver, and the sulfur hexafluoride gaseous component is exhaled through the lungs. The technique can be performed in patients with kidney failure and does not require previous laboratory tests. In addition, ultrasonic contrast agents (UCAs) have a lower risk of adverse reactions than contrast agents commonly used in computed tomography and magnetic resonance imaging. The CEUS is also inexpensive, fast, portable, repeatable, and safe with multiple injections, all without radiation exposure [20]. The arterial phase in CEUS is the most important tool of the examination. The testicle and epididymis enhance quickly, but it can vary from individual to individual. Arteries enhance first, followed in seconds by the reinforcement of the entire parenchyma. The scrotal wall tends to enhance lesser than the content. The enhancement decreases in a variable period usually 3 min. The normal testicular parenchyma is homogeneous with an echogenic surface line indicating the tunica albuginea. On CEUS, the testicle should enhance homogeneously with a striated pattern representing UCAs within the normal intratesticular vascular anatomy [20]. CEUS more clearly depicts the fracture lines, interruption of the tunica albuginea, and both intratesticular and extratesticular hematomas [21]. It can assess exact extent of viable testis, allowing the urologist to decide when the partial salvage of the organ is a good solution [22]. In addition, small testicular tumors may appear avascular in CDUS; thus, the differentiation of infarction can be difficult. CEUS can distinguish vascularized from non-vascularized focal testicular lesions, which help exclude malignancy. Finally, the Scrotal and Penile Imaging Working Group of the European Society of Urogenital Radiology provided position statements with the aim of guiding the use of imaging, especially multiparametric US, in scrotal trauma. Accordingly, CEUS can be used to identify the presence or absence of flow when CDUS is not diagnostic; identify testicular ruptures, fracture lines, hematomas, and ischemic changes in equivocal cases in conventional US; and distinguish between avascular and poorly vascularized lesions, to differentiate hematomas from tumors [23].
CONCLUSION
Scrotal US is the first-line imaging modality for the diagnosis of testicular trauma. Currently, CEUS is the first-line imaging modality for studying the traumatic pathology of the scrotum. CEUS has the potential to become an indispensable tool in the assessment of acute scrotal trauma, providing accurate and diagnostic imaging and helping increase the confidence of the doctor. The use of contrast media in US may be an optimal solution for a prompt resolution of equivocal US findings, combining the facility of US and information on the parenchymal vascularity offered by CEUS. This is particularly relevant for the surgical decision as to whether or not to undertake emergency surgery and, above all, whether the affected testicle is salvageable. The current management strategy for testicular rupture is surgical exploration and repair within 72 h to maximize the rescue.
ADDITIONAL INFORMATION
Funding source. This study was not supported by any external sources of funding.
Competing interest. Authors declare no explicit and potential conflicts of interests associated with the publication of this article.
Authors’ contribution. All authors made a substantial contribution to the conception of the work; acquisition, analysis, and interpretation of data for the work; drafting and revising the work; final approval of the version to be published; and agree to be accountable for all aspects of the work. L. Eusebi and M.T. Paparella contributed equally to the research work related to the topic and manuscript writing; A. Marconi helped in literature research and data acquisition; G. Guglielmi was involved in the critical revision of the manuscript.
Consent for publication. Written consent was obtained from the patient for the publication of relevant medical information and all accompanying images.
Авторлар туралы
Laura Eusebi
Radiology Unit, “Carlo Urbani” Hospital
Email: lauraeu@virgilio.it
ORCID iD: 0000-0002-4172-5126
Италия, Jesi
Maria Paparella
Department of Clinical and Experimental Medicine, Foggia University School of Medicine
Email: mt.paparella@gmail.com
ORCID iD: 0000-0003-2573-9509
Италия, Foggia
Andrea Marconi
Department of Urology, “Carlo Urbani” Hospital
Email: andreamarconi3@virgilio.it
Италия, Jesi
Giuseppe Guglielmi
Department of Clinical and Experimental Medicine, Foggia University School of Medicine; Radiology Unit, Barletta University Campus UNIFG, “Dimiccoli” Hospital
Хат алмасуға жауапты Автор.
Email: giuseppe.guglielmi@unifg.it
ORCID iD: 0000-0002-4325-8330
Medical Doctor, Full Professor of Radiology, Department of Clinical and Experimental Medicine.
Италия, Foggia; FoggiaӘдебиет тізімі
- Deurdulian C, Mittelstaedt CA, Chong WK, Fielding JR. US of acute scrotal trauma: optimal technique, imaging findings, and management. Radiographics. 2007;27(2):357–369. doi: 10.1148/rg.272065117
- Bhatt S, Dogra VS. Role of US in testicular and scrotal trauma. Radiographics. 2008;28(6):1617–1629. doi: 10.1148/rg.286085507
- Sadjo SA, Destinval C, Lemelle JL, Berte N. Testicular rupture after blunt scrotal trauma in children: a case report and literature review. Trauma Case Rep. 2021;33:100482. doi: 10.1016/j.tcr.2021.100482
- Wessells H, Long L. Penile and genital injuries. Urol Clin North Am. 2006;33(1):117–126. doi: 10.1016/j.ucl.2005.11.003
- Haas CA, Brown SL, Spirnak JP. Penile fracture and testicular rupture. World J Urol. 1999;17(2):101–106. doi: 10.1007/s003450050114
- Munter DW, Faleski EJ. Blunt scrotal trauma: emergency department evaluation and management. Am J Emerg Med. 1989;7(2):227–234. doi: 10.1016/0735-6757(89)90143-5
- Mulhall JP, Gabram SG, Jacobs LM. Emergency management of blunt testicular trauma. Acad Emerg Med. 1995;2(7):639–643. doi: 10.1111/j.1553-2712.1995.tb03604.x
- Huang DY, Pesapane F, Rafailidis V, et al. The role of multiparametric ultrasound in the diagnosis of paediatric scrotal pathology. Br J Radiol. 2020;93(1110):20200063. doi: 10.1259/bjr.20200063
- Wright S, Hoffmann B. Emergency ultrasound of acute scrotal pain. Eur J Emerg Med. 2015;22(1):2–9. doi: 10.1097/MEJ.0000000000000123
- Wang A, Stormont I, Siddiqui MM. A review of imaging modalities used in the diagnosis and management of scrotal trauma. Current Urology Reports. 2017;18(12):98–103. doi: 10.1007/s11934-017-0744-1
- Kitrey ND, Djakovic N, Gonsalves M, et al. EAU guidelines on urological trauma. European Association of Urology; 2016. Available from: https://uroweb.org/individual-guidelines/non-oncology-guidelines/
- Cannis M, Mailhot T, Perera P. Bedside ultrasound in a case of blunt scrotal trauma. West J Emergency Med. 2013;14(2):127–129. doi: 10.5811/westjem.2012.8.12630
- Bhatt S, Ghazale H, Dogra VS. Sonographic evaluation of scrotal and penile trauma. Ultrasound Clin. 2007;2(1):45–56. doi: 10.1016/j.cult.2007.01.003
- Pepe P, Panella P, Pennisi M, Aragona F. Does color Doppler sonography improve the clinical assessment of patients with acute scrotum? Eur J Radiol. 2006;60(1):120–124. doi: 10.1016/j.ejrad.2006.04.016
- Muttarak M, Thinyu S, Lojanapiwat B. Clinics in diagnostic imaging (114). Rupture of the right testis. Singapore Med J. 2007;48(3):264–268.
- Yusuf G, Konstantatou E, Sellars ME, et al. Multiparametric sonography of testicular hematomas: features on grayscale, color Doppler, and contrast-enhanced sonography and strain elastography. J Ultrasound Med. 2015;34:1319–1328. doi: 10.7863/ultra.34.7.1319
- Hedayati V, Sellars ME, Sharma DM, Sidhu PS. Contrast-enhanced ultrasound in testicular trauma: role in directing exploration, debridement and organ salvage. Br J Radiol. 2012;85(1011):e65–e68. doi: 10.1259/bjr/95600238
- Badea R, Lucan C, Suciu M, et al. Contrast enhanced harmonic ultrasonography for the evaluation of acute scrotal pathology. A pictorial essay. Med Ultrason. 2016;18(1):110–115. doi: 10.11152/mu.2013.2066.181.esy
- Sidhu PS, Cantisani V, Dietrich CF, et al. The EFSUMB guidelines and recommendations for the clinical practice of contrast-enhanced ultrasound (CEUS) in non-hepatic applications: update 2017 (short version). Ultraschall Med. 2018;39(2):154–180. doi: 10.1055/s-0044-101254
- Yusuf GT, Rafailidis V, Moore S, et al. The role of contrast-enhanced ultrasound (CEUS) in the evaluation of scrotal trauma: a review. Insights Imaging. 2020;11(1):68. doi: 10.1186/s13244-020-00874-7
- Trinci M, Cirimele V, Ferrari R, et al. Diagnostic value of contrast-enhanced ultrasound (CEUS) and comparison with color Doppler ultrasound and magnetic resonance in a case of scrotal trauma. J Ultrasound. 2020;23(2):189–194. doi: 10.1007/s40477-019-00389-y
- Valentino M, Bertolotto M, Derchi L, et al. Role of contrast enhanced ultrasound in acute scrotal diseases. Eur Radiol. 2011;21(9):1831–1840. doi: 10.1007/s00330-010-2039-5
- Ramanathan S, Bertolotto M, Freeman S, et al. Imaging in scrotal trauma: a European Society of Urogenital Radiology Scrotal and Penile Imaging Working Group (ESUR-SPIWG) position statement. Eur Radiol. 2021;31(7):4918–4928. doi: 10.1007/s00330-020-07631-w
Қосымша файлдар