类风湿性关节炎患者肩关节磁共振成像上的米粒体症状
- 作者: Ageeva S.F.1, Filatova D.A.1, Mershina E.A.1, Sinitsyn V.Е.1
-
隶属关系:
- Lomonosov Moscow State University
- 期: 卷 4, 编号 4 (2023)
- 页面: 616-624
- 栏目: 临床病例及临床病例的系列
- ##submission.dateSubmitted##: 26.06.2023
- ##submission.dateAccepted##: 05.09.2023
- ##submission.datePublished##: 15.12.2023
- URL: https://jdigitaldiagnostics.com/DD/article/view/508786
- DOI: https://doi.org/10.17816/DD508786
- ID: 508786
如何引用文章
详细
类风湿性关节炎患者肩关节磁共振成像(MRI)上的米粒体症状是一种罕见但特殊的发现。其特征是关节滑液、滑膜囊或滑膜鞘中出现多个圆形小结构。这些结构彼此相似,就像米粒一样。米粒体的成因至今不明。据推测,米粒体是因类风湿性关节炎或其他炎症性关节疾病患者滑膜微梗塞而形成的。在临床上,米粒体的存在可能会使患者感到疼痛。然而,情况并非总是如此。在放射诊断方法中,磁共振成像在检测米粒体方面发挥着主导作用。
本文介绍一例在肩关节磁共振成像中发现该症状的临床病例。该症状是在一名有长期类风湿性关节炎病史的患者身上发现的。患者因左肩部无痛性增大而就医。对左肩关节进行了电子计算机断层扫描(CT)和磁共振成像检查。医生通过这些检查发现了,米粒体症状是基础疾病的一种表现形式。这些检查有助于确定进一步的治疗策略。
全文:
背景
类风湿性关节炎(rheumatoid arthritis,RA)是一种以关节损伤和关节外表现为特征的慢性全身性自身免疫性疾病。这种疾病在女性中比较常见,通常在35-60岁发病(不包括幼年型类风湿性关节炎)[1-3]。
类风湿性关节炎在全球成年人口中的发病率相当高,从0.5%到2%不等。根据世界卫生组织的数据统计,2019年,类风湿性关节炎患者总数为1800万人[4]。截至2017年,俄罗斯正式登记的类风湿性关节炎患者有30.12万人;然而,根据俄罗斯流行病学研究,这种疾病影响约0.6%的普通人群[2]。
类风湿性关节炎的诊断基于临床和实验室检查结果以及放射治疗数据。根据2010年ACR-EULAR(American College of Rheumatology and the European League Against Rheumatism)标准,6分或6分以上(满分10分)表示患者存在类风湿性关节炎(表1)[2,5]。
表1。2010年American College of Rheumatology and the European League Against Rheumatism类风湿性关节炎诊断标准[2,5]
关节病变的临床表现(客观检查时出现肿胀和/或疼痛)(0–5分) | |
涉及1个主要关节 | 0分 |
涉及2–10个主要关节 | 1分 |
涉及1–3个小关节 | 2分 |
涉及4–10个小关节 | 3分 |
涉及10个以上关节,其中至少有1个小关节 | 5分 |
实验室方法检测RF和抗CCP抗体的结果(0–3分,要求至少一种方法的阳性结果) | |
RF——阴性,抗CCP抗体——阴性 | 0分 |
RF——弱阳性或抗CCP抗体——弱阳性(超出正常值上限,但不超过3倍) | 2分 |
RF——高危阳性或抗CCP抗体——高危阳性(超过正常值上限3倍以上) | 3分 |
实验室方法检测“急性期”指标的结果(0–1分,要求至少一种方法的阳性结果) | |
正常ESR值和正常CRP值 | 0 分 |
ESR升高或CRP升高 | 1 分 |
关节炎持续时间(0–1分) | |
<6个月 | 0分 |
�6个月 | 1分 |
注:RF(rheumatoid factor)——类风湿因子;抗CCP抗体——抗环瓜氨酸肽抗体;ESR(erythrocyte sedimentation rate)——红细胞沉降率;CRP(C-reactive protein)——C反应蛋白。
类风湿性关节炎最主要的临床表现如下:
- 关节痛;
- 受影响关节的早上起来僵硬(超过30分钟);
- 发热;
- 皮下出现类风湿结节;
- 虚弱;
- 体重减轻。
通常,小关节(近端指间关节、掌指关节)首先会对称受累。然后,随着病情的发展,较大的关节也会受到影响。该病可能有肺部、肾脏、心血管和皮肤表现[1–3]。
X射线方法被广泛用于诊断和评估类风湿性关节炎病程的动态变化。它们可以检测和评估影响肌肉骨骼系统的 类风湿性关节炎表现和关节外表现(呼吸系统、心脏的病变,费尔蒂综合征中脾肿大的存在)。
磁共振成像(MRI)目前被常用于评估关节疾病的表现。这种方法具有较高的软组织分辨率,因此可以发现疾病的早期表现(如滑膜炎、糜烂、软骨损伤)[6]。
在某些类风湿性关节炎病例中,滑液、滑膜囊或阴道中可能会出现米粒样的小结构,即所谓的“米粒体”。这些结构呈圆形、多发、体积小、彼此相似,类似米粒,因此得名。从组织学角度看,它们由嗜酸性无定形核组成,表面被纤维蛋白和胶原蛋白覆盖[7,8]。“米粒体”的确切病因尚不清楚。有人认为,它们的出现是由于关节滑膜发生微损伤,导致小颗粒脱落和分离,其表面随后被纤维蛋白覆盖。人们认为“米粒体”可能与关节炎症有关。它们通常出现在类风湿性关节炎中,但也可能出现在结核性关节炎、慢性滑囊炎和滑膜炎以及其他一些疾病中。临床上,这种综合征可能表现为疼痛,也可能没有症状[3,9]。磁共振成像是检测“米粒体”的最佳方法[9,10]。
病例介绍
患者I,59岁,有长期的类风湿性关节炎病史。2022年9月,由于左肩关节无痛性增大,她来到诊所接受磁共振成像检查。
病史
2015年,患者被诊断出患有类风湿性关节炎,首发症状表现为左膝关节和足部关节炎。根据ACR-EULAR标准,患者在类风湿性关节炎量表中的评分为10分中的7分(可靠诊断需要大于6分)。
2017年确诊为桥本甲状腺炎。
2021年,患者因书写严重困难而去看风湿病专家。根据2021年2月磁共振成像的描述(在另一家机构进行),患者的两个肩关节均有损伤:
- 三角肌下和肩峰下囊可见大量渗液,右侧更为明显;
- 关节滑膜增厚,关节腔内有少量渗液;
- 关节软骨表面的信号减弱。
实验诊断
2022年9月16日,为了评估正在进行的治疗(甲氨蝶呤为17.5mg、叶酸),进行了血液检测:
- 甲状腺激素——正常:4.08µIU/ml(正常值为0.27-4.2µIU/ml);
- 类风湿因子——升高:107.9IU/ml(正常值为0-14IU/ml);
- C反应蛋白——升高:11.84mg/L(正常值为0-5mg/L);
- 红细胞沉降率——升高:36mm/h(正常值小于30mm/h)。
仪器诊断
2022年9月17日,患者接受了双肩关节CT扫描检查和左肩关节磁共振成像检查,原因是根据患者的主诉,左肩关节的体积进一步增大。
磁共振成像是在3T磁场MR系统(MAGNETOM Vida,Siemens Healthineers,德国)上进行,采用标准方案(T1和T2加权图像,用或不用脂肪抑制,横向、正面、矢状和斜向切片),并配有肩部表面射频线圈。
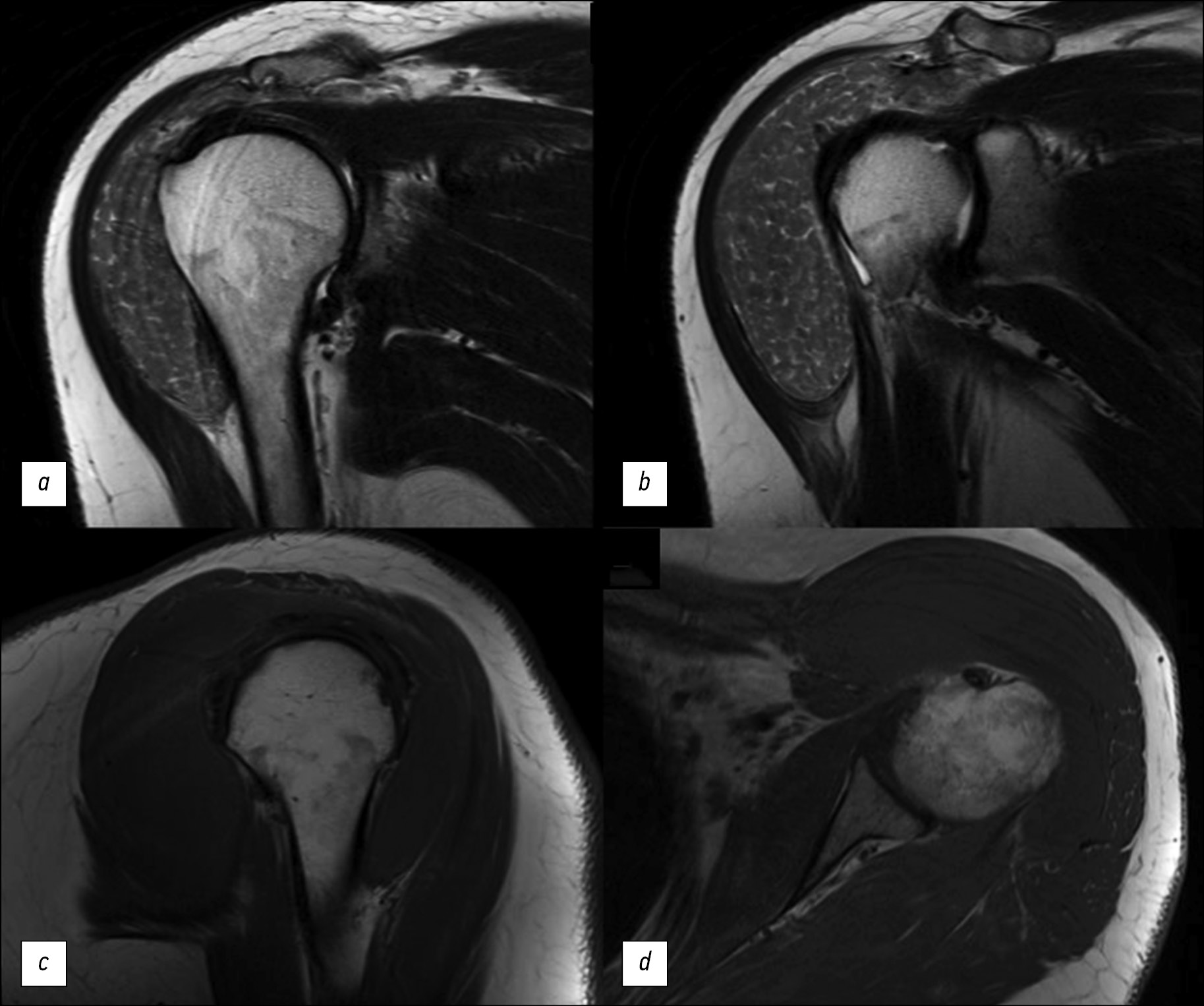
在三角肌下的T2加权图像上,在肿大至7.7×2.5×5cm的肩峰下和三角肌下滑膜囊内部,发现了许多类似的小椭圆形结构,信号强度中等,直径从2-3mm到8-10mm不等,被信号增强区域(在T2加权图像上)分隔。在T1加权图像上,它们的信号强度处于中等水平,且均匀一致(图1、图2)。这些小体团看起来就像是在关节腔内形成的一个占位性肿块。
图1。左肩关节磁共振成像:a、b——T2加权图像,冠状切片;c——T1加权图像,矢状切片;d——T1加权图像,横向切片。
图2。左肩关节磁共振成像,脂肪信号抑制的T2加权图像:a——横向切片;b——正面切片。滑膜囊内的小结构用箭头表示。
在Somatom Drive断层扫描仪(Siemehns Healthineers,德国)上对肩关节进行了CT扫 描(无对比剂),切片厚度为0.625mm,结果发现两侧肩峰下和三角肌下囊均有大尺寸的透镜状低密度结构(图3):
- 左侧: 7.5×4×9cm;与MR评估(7.7×2.5×5cm)相比,肿块的尺寸更大;
- 右侧: 4×4×4cm。
图3。肩关节计算机断层扫描,轴向切片:a——左肩关节,b——右肩关节。
它们在CT图像上的结构均匀,没有钙化物和致密包体,密度约为35HU。双侧腋窝反应性淋巴结肿大与主要疾病相关。
讨论
关节内“米粒体”症状是一种与关节炎症有关的罕见现象。它在类风湿性关节炎患者中最为常见。这些肿块可能是类风湿性关节炎的一种表现,也可能在疾病发展之前出现(在极少数情况下)[11]。“米粒体”可能没有症状,也可能表现为受累关节肿大(如上述病例)和疼痛。
在MR检查中,“米粒体”看起来像多个大小相似的圆形肿块。它们在T1加权图像上呈等或低密度信号,在T2加权图像上呈低密度信号。对上述病例来说,在T2加权图像上,“米粒体”密集排列,与肌肉相对密集,这是类风湿性关节炎的唯一病理特征。此外,正如本病例所示,磁共振成像在检测这些结构方面比CT更有优势。
重要的是要记住,“米粒体”不仅可以在类风湿性关节炎中观察到,也可以在其他疾病中观察到,包括滑膜软骨瘤病和色素沉着绒毛结节性滑膜炎、慢性滑囊炎,包括结核病因。磁共振成像大大方便了这些疾病的鉴别诊断。在第一种疾病的病例中,T1加权图像上的等或高强信号、T2加权图像上高强液体背景下“米粒体”的低强信号均出现在软骨组织区域。此外,对男性来说,滑膜软骨瘤病更为常见,而且是单关节的。在色素沉着绒毛结节性滑膜炎患者中,由于含铁血黄素沉积,T1加权图像和T2加权图像上不均匀增厚的滑膜信号减弱[8]。
由于纤维蛋白具有刺激作用,“米粒体”本身会刺激滑膜炎症。手术干预被认为会对患者的临床状况产生有利影响[12, 13],尤其是在剧烈疼痛的情况下。在这种情况下,对患者的进一步治疗建议采用手术治疗。
结论
本文描述了一例罕见的关节内“米粒体”综合征临床病例,患者有长期的类风湿性关节炎病史。本文给出有关该主题的文献综述,并描述该病理的MR和CT征象。
虽然“米粒体”是一种罕见的病理现象,但我们仍有必要记得其在类风湿性关节炎患者关节囊中的存在,并将其与其他病因引起的类似病理结果区分开来。
ADDITIONAL INFORMATION
Funding source. This article was not supported by any external sources of funding.
Competing interests. The authors declare that they have no competing interests.
Authors’ contribution. All authors made a substantial contribution to the conception of the work, acquisition, analysis, interpretation of data for the work, drafting and revising the work, final approval of the version to be published and agree to be accountable for all aspects of the work. S.F. Ageeva — writing the text; D.A. Filatova — writing and reviewing the text; E.A. Mershina — concept development, approval of the final text; V.E. Sinitsyn — concept development, approval of the final text.
Consent for publication. Written consent was obtained from the patient for publication of relevant medical information and all of accompanying images within the manuscript in Digital Diagnostics Journal.
作者简介
Sofia F. Ageeva
Lomonosov Moscow State University
编辑信件的主要联系方式.
Email: son.ageeva13@gmail.com
ORCID iD: 0000-0003-4726-0806
SPIN 代码: 9695-3717
俄罗斯联邦, Moscow
Daria A. Filatova
Lomonosov Moscow State University
Email: dariafilatova.msu@mail.ru
ORCID iD: 0000-0002-0894-1994
SPIN 代码: 2665-5973
俄罗斯联邦, Moscow
Elena A. Mershina
Lomonosov Moscow State University
Email: elena_mershina@mail.ru
ORCID iD: 0000-0002-1266-4926
SPIN 代码: 6897-9641
MD, Cand. Sci. (Med.), Аssistant professor
俄罗斯联邦, MoscowValentin Е. Sinitsyn
Lomonosov Moscow State University
Email: vsini@mail.ru
ORCID iD: 0000-0002-5649-2193
SPIN 代码: 8449-6590
MD, Dr. Sci. (Med.), Professor
俄罗斯联邦, Moscow参考
- Nasonov EL, Karateev DE, Balabanova RM. Rheumatoid arthritis. In: Nasonov EL, Nasonova VA, editors. Rheumatology. National manual. Moscow : GEOTAR-Media. 2008. P. 290–331 (In Russ)
- Rheumatoid arthritis. Clinical Guidelines. ID 250. Approved by the Scientific and Practical Council of the Ministry of Health of the Russian Federation. 2021. Available from: https://cr.minzdrav.gov.ru/schema/250 (In Russ)
- Bullock J, Rizvi SA, Saleh AM, et al. Rheumatoid Arthritis: A Brief Overview of the Treatment. Medical Principles and Practice. 2018;27(6):501–507. doi: 10.1159/000493390
- who.int [Internet]. World Health Organization [cited 6 September 2023]. Available from: https://www.who.int
- Kay J, Upchurch KS. ACR/EULAR 2010 rheumatoid arthritis classification criteria. Rheumatology. 2012;51 Suppl. 6:vi5–vi9. doi: 10.1093/rheumatology/kes279
- Narvaez JA, Narváez J, De Lama E, et al. MR Imaging of Early Rheumatoid Arthritis. RadioGraphics. 2010;30(1):143–163. doi: 10.1148/rg.301095089
- Edison MN, Caram A, Flores M, et al. Rice Body Formation Within a Peri-Articular Shoulder Mass. Cureus. 2016;8(8):e718. doi: 10.7759/cureus.718
- Forse CL, Mucha BL, Santos MLZ., et al. Rice body formation without rheumatic disease or tuberculosis infection: a case report and literature review. Clinical Rheumatology. 2012;31(12):1753–1756. doi: 10.1007/s10067-012-2063-8
- Narváez JA, Narváez J, Roca Y, et al. MR imaging assessment of clinical problems in rheumatoid arthritis. European Radiology. 2002;12(7):1819–1828. doi: 10.1007/s00330-001-1207-z
- Griffith JF, Peh WCG, Evans NS, et al. Multiple rice body formation in chronic subacromial/subdeltoid bursitis: MR appearances. Clinical Radiology. 1996;51(7):511–514. doi: 10.1016/s0009-9260(96)80193-0
- Kataria RK, Chaiamnuay S, Jacobson LD, et al. Subacromial bursitis with rice bodies as the presenting manifestation of rheumatoid arthritis. The Journal of rheumatology. 2003;30(6):1354–1355.
- Popert AJ, Scott DL, Wainwright AC, et al. Frequency of occurrence, mode of development, and significance or rice bodies in rheumatoid joints. Annals of the Rheumatic Diseases. 1982;41(2):109–117. doi: 10.1136/ard.41.2.109
- Reid HS, McNally E, Carr A. Soft tissue mass around the shoulder. Annals of the Rheumatic Diseases. 1998;57(1):6–8. doi: 10.1136/ard.57.1.6
补充文件