Evaluation of fetal absorbed doses from computed tomography examinations of pregnant patients: A systematic review
- Authors: Vodovatov A.V.1, Golchenko O.A.2, Mashchenko I.A.3, Alekseeva D.V.3, Chipiga L.A.1,3, Khutornoy I.V.4, Kozlova P.V.3, Trufanov G.E.3, Druzhinina P.S.1, Ryzhov S.A.5, Soldatov I.V.5
-
Affiliations:
- Saint-Petersburg Research Institute of Radiation Hygiene after Professor P.V. Ramzaev
- City polyclinic № 19
- Almazov National Medical Research Centre
- Lomonosov Moscow State University
- Research and Practice Center of Diagnostics and Telemedicine Technologies
- Issue: Vol 4, No 2 (2023)
- Pages: 170-184
- Section: Systematic reviews
- Submitted: 05.06.2023
- Accepted: 19.06.2023
- Published: 12.07.2023
- URL: https://jdigitaldiagnostics.com/DD/article/view/472150
- DOI: https://doi.org/10.17816/DD472150
- ID: 472150
Cite item
Abstract
BACKGROUND: Currently, no systematic data are available on fetal radiation exposure as a result of radiographic studies during pregnancy. Consequently, there are no approved methods of its calculation that can be used in clinical practice. It is especially relevant for computed tomography scans as it is a widely used and highly informative method of diagnostic imaging associated with high exposure levels.
AIM: to systematize currently available data on radiation dose absorbed by the fetus from computed tomography scans in pregnant women.
MATERIALS AND METHODS: The search for publications in Russian and English was conducted in PubMed/Medline, Google Scholar and еLibrary. The final analysis included 12 papers including 8 studies using human body phantoms, 3 retrospective studies and one prospective clinical study.
RESULTS: Abdominal and pelvic computed tomography scans as well as whole-body scans were found to be associated with the highest fetal radiation exposure. However, in none of the publications the fetal exposure limit was exceeded.
CONCLUSION: Clinically indicated non-contrast-enhanced computed tomography scans in pregnant women are not likely to be associated with the fetal absorbed doses that exceed the limit of 100 mGy regardless of the scanned area. However, this limit might be exceeded in case of performing multiple studies or if multiphase abdominal or pelvic computed tomography scans, or whole-body computed tomography scans are performed in patients with multiple trauma. In these cases, a decision regarding the need for these investigations should be made by a multi-disciplinary team (including radiation safety specialists, diagnostic radiologists and clinicians) based on the results of additional risk assessment.
Full Text
BACKGROUND
During pregnancy, the safety of diagnostic radiology is a priority for radiologists and other specialists. Until the middle of the 20th century, medical imaging methods using ionizing radiation sources were widely used in obstetrics for diagnostic and therapeutic purposes. However, later experimental and epidemiological data on the effects of ionizing radiation on fetal development were obtained. The International Commission on Radiation Protection established limitations for the use of ionizing radiation during pregnancy [1].
The negative effects of ionizing radiation are usually classified into deterministic and stochastic effects. Deterministic effects are associated with direct cell damage or death resulting from radiation exposure above the threshold level. The probability of these effects depends on the radiation dose and gestational age of the fetus. The main fetal risks include congenital malformations of the internal organs and central nervous system (such as neurological disorders and developmental delays). The severity of the deterministic effects is proportional to the dose and frequency of examinations.
Fetal sensitivity to radiation depends on the gestational age of the fetus. Organogenesis (pregnancy weeks 5–17 or post-conception weeks 3–15) is the most dangerous period for radiation exposure. In the second and third trimesters, fetal resistance to radiation increases; however, in this period, exposure to >500 mGy can still lead to adverse effects, including growth retardation and malformations [2].
Currently, the no-effect threshold value of the fetal absorbed dose is 100 mGy [3, 4]. International professional societies (International Commission on Radiation Protection, U.S. National Council on Radiation Protection, American College of Radiology, and American College of Obstetricians and Gynecologists) consider the risk of spontaneous abortion and serious malformations to be negligible in fetuses exposed to radiation doses <50 mGy [3-6].
Stochastic effects are radiation-induced changes in cells that can lead to malignant neoplasms. Stochastic effects do not have a threshold, and data on the corresponding risk are inconsistent [7]. According to the clinical practical guidelines of the American College of Radiology, an absorbed fetal dose of 20 mGy corresponds to a cancer risk of 1/125 in addition to background incidence [6]. According to the International Commission on Radiation Protection, the fetal cancer risk is lower and is 1/500 at the fetal absorbed dose of 30 mGy. In Russian research practice, the risk of radiation-induced cancers and genetic fetal effects following medical radiation exposure have not been examined [8].
Improvements in medical imaging techniques have led to their widespread application and use in the differential diagnosis of some life-threatening conditions, which requires an assessment of their safety in pregnancy. A quantitative evaluation of fetal radiation exposure level is the most reliable assessment of the safety profile of medical imaging techniques in pregnancy. Moreover, pathological conditions that most often require various imaging studies in pregnant patients must be assessed, such as pulmonary embolism (PE), aortic dissection, polytrauma, urolithiasis, acute appendicitis, and lung damage in COVID-19 [9–12].
Fetal safety is the main parameter for imaging technique selection in pregnant women [6]. To reduce potential risks of negative effects, pregnant patients should be protected from radiation using recommended means. Unfortunately, in Russian practice, no such recommendations have been established, and no Russian data on fetal exposure doses when using certain medical imaging techniques are available [8]. Thus, the authors conducted this systematic review to summarize and analyze current data on fetal radiation exposure levels when using computed tomography (CT), the highest-dose imaging technique.
MATERIALS AND METHODS
Study design
The systematic review was based on PRISMA guidelines (2009).
Literature search
Study materials included scientific publications searched from PubMed/Medline, Google Scholar, and eLibrary databases. Existing foreign and national guidelines for imaging studies in pregnancy were also reviewed. The following keywords were used: CT, pregnancy, radiation risk, organ dose, diagnostic imaging, fetal risks pregnancy radiation, computed tomography, and fetal absorbed doses.
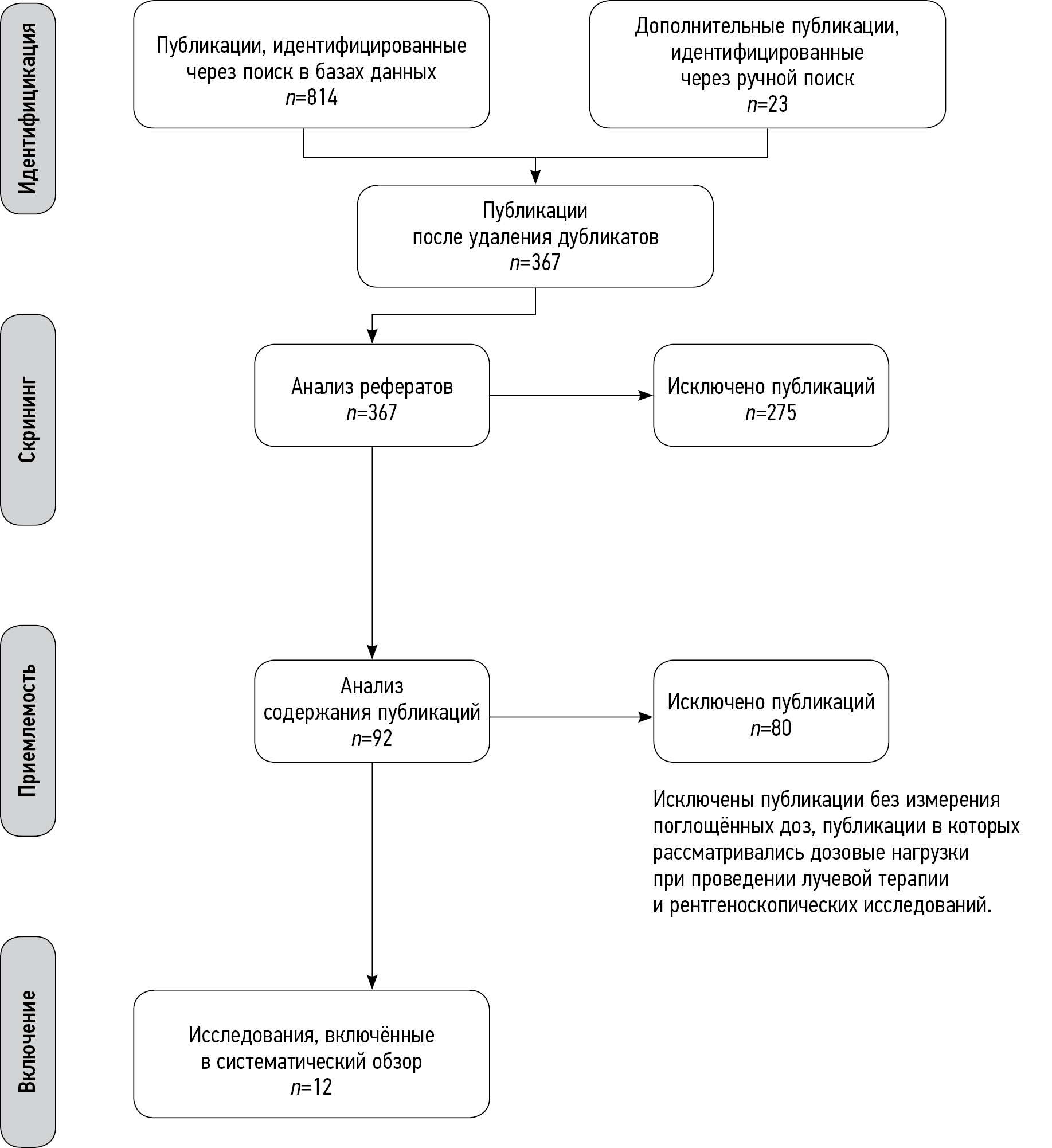
Following the database search query, duplicate results were excluded. The content of the selected studies, including parameters such as the year of publication, study design, purpose, methodology, and results were analyzed, and publications on non-ionizing techniques of diagnostic radiology were excluded. The systematic review excluded studies that did not measure fetal and uterus absorbed doses and studies measuring dose loads during radiation therapy and fluoroscopy. Finally, the systematic review included 12 studies. The study design is presented in Fig. 1.
Fig. 1. Study design in the PRISMA scheme.
Estimated parameters
The systematic review evaluated selected publications using the following parameters: doses absorbed by the fetus/embryo, gestational age, pathological condition, anatomical area of interest, method of absorbed dose estimation, and number of studied cases using CT in pregnant women. The systematic review included clinical and experimental studies using anthropomorphic phantoms.
RESULTS
In total, 837 studies were found in PubMed/Medline, Google Scholar, and eLibrary databases for the following search queries: “CT radiation risk in pregnancy,” “fetal absorbed doses from diagnostic imaging,” “CT fetal dosimetry,” and “assessment of fetal doses in CT” from 2007 to 2022. After a preliminary analysis and removal of duplicate results, 12 studies in English and Russian were included in the review, including 8 studies using anthropomorphic phantoms, 3 retrospective studies, and 1 prospective clinical study. Each study was evaluated by the study type and design, measurement method, and calculation method of absorbed doses. Information on studies is summarized in Tables 1–7.
Table 1. Characteristics of studies using anthropomorphic phantoms
Source | Method for measuring doses | Estimated absorbed doses |
Angel et al. 2008 [15] | Not reported | ImPACT; MC; CT Expo |
Begano et al. 2020 [33] | TLD | VirtualDose CT |
Doshi et al. 2008 [36] | TLD | According to TLD measurements |
Kelaranta et al. 2017 [14] | MOSFET | ImPACT MC |
Vodovatov et al. 2021 [8] | Not reported | NCICT3.0 |
Gilet et al. 2011 [37] | TLD | According to TLD measurements |
Gu et al. 2009 [13] | MOSFET | MCNPX According to MOSFET measurements |
Jaffe et al. 2008 [26] | MOSFET | According to MOSFET measurements |
Note. MOSFET, metal oxide semiconductor field-effect transistor; TLD, thermoluminescent dosimeter.
Table 2. Characteristics of clinical studies
Paper | Type of study | Estimated absorbed doses |
Lazarus et al. 2009 [29] | Retrospective clinical study | Not reported |
Goldberg-Stein et al. 2011 [16] | Retrospective clinical study | ImPACT |
Litmanovich et al. 2009 [32] | Prospective clinical study | ImPACT |
Lazarus et al. 2007 [30] | Retrospective clinical study | Not reported |
Table 3. Protocols of CT for anthropomorphic phantoms
Source | CT machine model | Voltage, kV | Exposure, mAs | Pitch factor | Gestational age, weeks | Scan length, cm |
Angel et al. 2008 [15] | LightSpeed 16, GE | 120 | 100–300 | 1,375 | 5–36 | 46,2 |
Begano et al. 2020 [33] | Definition Flash CT (Siemens Healthineers,Germany) | 120 | 85 | 1,5 | 28–38 | 32 cm, standard program; 22 cm, short program |
Doshi et al. 2008 [36] | Siemens Sensation 16 Siemens Somatom Emotion / Marconi MX8000 | 100–130 | 125–250 | 1,25 | 35–40 | 32 cm, standard program; 27 cm, short program |
Gilet et al. 2011 [37] | LightSpeed 4 LightSpeed 16 LightSpeed 64 VCT, GE Healthcare | 120 | 100–500 | 1,375–1,5 | 5, 10, 18, 32 | 32 |
Gu et al. 2013 [13] | LightSpeed 16 GE-MDCT | 80–140 | 100 | 1,375 | 15,20,31 | 22 cm, ches; 36 cm, abdomen |
Kelaranta et al. 2017 [14] | LightSpeed 64-MDCT GE | 100–120 | 100–300 | 1,375 | 12, 20, 28, 38 | 27 cm, chest; 32 cm, abdomen; 94 cm, trauma |
Vodovatov et al. 2021 [8] | Ingenuity 128, Philips Somatom Definition AS, Siemens Somatom Scope, Siemens Emotion 16, Siemens | 100–130 | 60–142 | 1,048–1,5 | 8, 10, 12, 15, 20, 25, 30, 35, 38 | 33 |
Jaffe et al. 2008 [26] | GE LightSpeed 16-MDCT | 140 | 300–380 | 0,9–1,75 | 5 | 32 |
Table 4. Protocols of CT for pregnant women
Source | CT machine model | Voltage, kV | Exposure, mAs | Pitch factor | Gestational age, weeks | Scan region (anatomical landmarks) |
Lazarus et al. 2007 [30] | Either single-detector row scanner (CTI GE Healthcare, Waukesha, WI), 4 MDCT Lightspeed; GE Healthcare) 16-MDCT Somatom; Siemens, Malvern | 140 | - | - | 5–40 | Abdomen |
Lazarus et al. 2009 [29] | - | - | - | - | - | Head Chest Abdomen and pelvis |
Litmanovich et al. 2009 [32] | 64-MDCT LightSpeed VCT | 100 | 200 | 0,984 | 5–36 | Chest Aortic arch to the diaphragmatic cupula 19.846 ± 2.98 cm |
Goldberg-Stein et al. 2011 [16] | LightSpeed Plus, LightSpeed 16 Pro, LightSpeed Qx/I, HighSpeed RP,HighSpeed CT/GE Healthcare) | 120–140 | 180–716 | 0,9–1,5 | 5–36 | Abdomen and pelvis |
Table 5. Systematized data on the assessment of fetal absorbed doses in chest CT
Source | Volume CT dose index (CTDI vol), mGy | DLP, mGy×cm | Gestational age, weeks | Fetal absorbed dose, mean, mGy | Uterus absorbed dose, mean, mGy |
In phantom studies | |||||
Kelaranta et al. 2017 [14] | 1,34–1,97 | 476,63– 582,22 | 12 20 28 38 | 0,03 0,08 0,14 0,22 | 0,04 0,09 0,29 1,13 |
Doshi et al. 2008 [36] | - | - | 35–40 | 0,23 | - |
Begano et al. 2020 [33] | 1,5–4,0 | 44–137 | 28–38 | 0,02–0,12 | - |
Gilet et al. 2011 [37] | - | - | 5–32 | 0,33–0,77 | - |
Gu et al. 2013 [13] | 8,1–14,7 | - | 15 20 31 | 0,13 0,21 0,26 | 0,17 0,33 0,37 |
Vodovatov et al. 2021 [8] | 5,6–9,3 | 185–306 | 8 10 15 20 25 30 35 38 | 0,09 0,10 0,08 0,13 0,12 0,16 0,39 0,52 | 0,09 0,10 0,07 0,09 0,11 0,15 0,33 0,64 |
In clinical studies | |||||
Litmanovich et al. 2009 [32] | 5,21 | 105,65 | 5–38 | 0,02 | - |
Lazarus et al. 2009 [29] | - | - | 1st, 2nd, and 3rd trimesters | 0,22 | - |
Note. CTDI, computed tomography dose index; DLP, dose–length product.
Table 6. Systematized data on the assessment of fetal absorbed doses in abdominal and pelvic CT
Source | Volume CT dose index (CTDI vol), mGy | DLP, mGy×cm | Gestational age, weeks | Fetal absorbed dose, mean, mGy | Uterus absorbed dose, mean, mGy |
In phantom studies | |||||
Kelaranta et al. 2017 [14] | 2,63–3,91 | 102,34–151,86 | 12 20 28 38 | 4,7 5,5 4,8 4,8 | 5,1 5,8 4,9 5,1 |
Angel et al. 2008 [15] | - | - | 5 12 15 20 25 30 35 | - 14,2 11,2 8,5 12,3 9,7 10,4 | 11,8 |
Gu et al. 2013 [13] | - | - | 15 | 6,9 | - |
Gilet et al. 2011 [37] | - | - | 5, 10, 18, 32 | 15–20,5 | - |
In clinical studies | |||||
Lazarus et al. 2009 [29] | - | - | 1st, 2nd, and 3rd trimesters | 17,1 | - |
Lazarus et al. 2007 [30] | - | - | 5–40 | 16 | - |
Goldberg-Stein et al. 2011 [16] | - | - | 5–36 | 24,8 | - |
Note. CTDI, computed tomography dose index; DLP, dose–length product.
Table 7. Systematized data on the assessment of fetal absorbed doses in CT for trauma in phantom studies
Source | CTDI, mGy | DLP, mGy×cm | Gestational age, weeks | Fetal absorbed dose, mean, mGy | Uterus absorbed dose, mean, mGy |
Kelaranta et al. 2017 [14] | 4,74–5,79 | 45,18–66,52 | 12 20 28 38 | 10,6 11,2 10,1 9,9 | 11,3 12,6 10,3 10,7 |
Jaffe et al. 2008 [26] | 6,55–26,02 | - | 5 | 18,0 | - |
Measurement and calculation of absorbed doses
Absorbed doses were measured using a thermoluminescent dosimeter (TLD) or metal oxide semiconductor field-effect transistor (MOSFET). In 2 of 8 studies, a virtual phantom technology was used, which involves mathematical modeling of the absorbed doses.
Absorbed doses were estimated based on measurement results or using special software for assessing absorbed doses in radiosensitive organs and tissues (ImPACT MC, CT EXPO, NCICT 3.0, and virtual dose CT).
In 2 of 4 clinical studies, absorbed doses were calculated using the special calculation program ImPACT. Two other studies did not provide information on calculation methods.
The gestational age modeled in anthropomorphic phantoms ranged from 5 to 40 weeks. In 5 of 8 studies, the scan length was 32 cm, which corresponds to the length of a standard phantom. In four studies, programs with decreased scan length were also used, and three studies used programs with increased scan length.
Comparative analysis
The fetal absorbed doses were compared in several groups by anatomical scan regions including chest, abdomen, pelvis, and whole body in trauma (Tables 5–7).
Considering the presented data of phantom studies, two pairs of studies were combined (Vodovatova et al. [8] and Gu et al. [13], and Kelaranta et al. [14] and Angel et al. [15]) to determine general patterns in absorbed dose change depending on the gestational age and scan region. In these studies, the gestational age and scan regions were comparable (chest in studies by Vodovatova and Gu, and abdomen or pelvis in studies by Kelaranta and Angel), and similar technical scan parameters (exposure, pitch factor, and voltage) were reported. The comparable nature of the above data made it possible to compare pooled data. The results of the comparative analysis are presented in Fig. 2. Chest scan showed a significantly lower fetal absorbed dose than the abdominal scan. In addition, in chest CT, the fetal absorbed dose tends to decrease slightly with increases in gestational age. To confirm these findings, more powerful studies are needed.
Fig. 2. Summary results of fetal dosimetry in chest CT (led by Vodovatov [8] and Gu [13]) and abdominal CT (led by Kelaranta [14] and Angel [15]) with LOESS regression line modeling and 95% confidence interval.
Finally, evidence suggests that the fetal absorbed dose threshold of 100 mGy [3, 5] indicated in regulatory and methodological documents significantly exceeds the observed levels of fetal exposure during phantom studies. Moreover, exposure levels of 20 and 30 mGy [5, 6], potentially leading to stochastic effects, are not achieved in single-phase CT on a once-only basis.
In all clinical studies included in the systematic review (except for the study by Goldberg-Stein et al. [16]), the fetal absorbed doses also did not exceed the above range of 20–100 mGy. In the study by Goldberg-Stein et al. [16], scan parameters were overestimated (up to 140 kV and 815 mAs), which led to a high fetal absorbed dose. Moreover, multiphase CT and multiple examinations were considered (highlighted in the text of the publication).
This comparison allows radiologists to conduct one single-phase CT in eligible pregnant women without undue concerns. If repeated scans are necessary, additional risk assessment shall be performed.
DISCUSSION
The main approaches to radiation safety in pregnant women are similar to those in other populations. In general, if ultrasound and magnetic resonance imaging are impossible to use as diagnostic techniques, ionizing radiation techniques should be used only in life-threatening situations with minimized radiation doses [17]. Life-threatening complications requiring diagnosis of pathological conditions should exceed the potential negative effect of diagnostic techniques. The choice of imaging techniques should be regulated in clinical standards of care with recommendations for their use in established or suspected diseases.
For the safe use of ionizing diagnostic techniques, the level of fetal absorbed doses must be monitored during the examination, and duplicate studies should not be conducted whenever appropriate [18].
CT is the most conclusive ionizing technique of diagnostic radiology. CT has an undeniable advantage such as short examination time combined with high informative value, making CT an optimal method for diagnosing life-threatening conditions that require immediate treatment [19, 20]. Depending on the indication and diagnostic goals, CT may be performed either as a native or a contrast-enhanced examination. Native examinations can be used in pregnant women to diagnose inflammatory lung diseases, urolithiasis, various traumatic injuries, etc. [21, 22]. Contrast-enhanced examination is necessary for differential diagnosis of neoplasms, inflammatory changes, and CT angiography for diagnosing thrombosis and vascular wall damage and assessing blood supply to certain structures [19, 23]. In pregnant patients, only one of these options must be selected. If contrast-enhanced CT is necessary, a native examination must be excluded to reduce the procedure time and radiation dose.
In diagnostic imaging of pregnant patients, the fetal absorbed dose must be assessed [24]. Owing to the limited capabilities of cohort studies on this issue, physical (anthropomorphic) or digital phantoms are currently widely used [25]. However, phantom studies using human body simulators have some limitations. They are mainly related to differences in phantom sizes and real patients. If real body parameters exceed the parameters of the phantom used, the absorbed dose will be overestimated, and vice versa, the dose may be underestimated if the patient’s dimensions are smaller than the dimensions of the phantom [25]. However, phantom studies are reasonable for use as experimental guidance because they provide more information on absorbed doses to be calculated for each week of pregnancy, in contrast to cohort studies, which provide calculation results as averaged doses. In addition, fetal absorbed doses in cohort and phantom studies were not significantly different (Tables 5–7).
Radiation doses directly depend on the scan region. When the fetus is outside the radiation field (CT region), it is exposed to scattered radiation. Therefore, the farther the scan region is located from the fetus, the lower the absorbed dose and the likelihood of negative effects [14].
The literature review showed that fetal absorbed doses directly correlated with the anatomical scan region. As shown in Tables 5–7, the maximum fetal absorbed doses are observed during CT of the whole body, abdomen, and pelvis. The lowest fetal absorbed doses are observed in chest CT. The estimated absorbed doses for phantoms are comparable with those obtained in cohort studies.
None of the foreign studies included in the review reported a fetal absorbed dose threshold exceeding 100 mGy. In Russia, no studies were conducted to evaluate indications for CT and the number of absorbed doses in pregnant women and fetuses during abdominal and pelvic CT.
In early gestation, the fetal absorbed dose assessment is difficult because of the small size of the embryo. Some studies [8, 26, 27] have shown insignificant differences in doses absorbed by the uterus and fetus. Therefore, the uterus absorbed dose can be used as an equivalent of the fetal absorbed dose [28]. Experimental studies have shown a relationship between the absorbed dose and gestational age.
Since the reviewed cohort studies presented data as average fetal absorbed doses for different gestational ages, determining the correlation between the gestational age and the level of absorbed dose is impossible for these studies [29–31].
In addition to the gestational age and anatomical scan regions, the absorbed dose depends on technical parameters such as the length of the scan region, algorithm for automatic modulation of the current strength, if any, pitch factor, and voltage.
The radiation dose can be decreased by changing the parameters of the scanning protocol and reducing the length of the scan region. In the study by Litmanovich et al. [32], 26 pregnant women with suspected PE underwent CT angiography of the pulmonary artery with decreased voltage and current and decreased scan length compared with the standard protocol. The effective dose was significantly lower than that in the control group (1.8 and 9.8 mSv, respectively) without a decrease in the diagnostic quality of the examination.
The decreased length of the scan region has also shown its effectiveness in phantom studies [33]. The authors reported a significant decrease in the mean fetal absorbed dose compared with doses for the standard scan length (0.03 and 0.1 mSv, respectively). However, some risks are associated with excluding part of anatomical structures from the scan region, and this should be considered when reducing the scan length.
Some studies have also considered the need to use screens (personal protective equipment) when conducting radiological examinations during pregnancy [33, 34]. The reviewed publications did not use additional protective measures when examining organs located at some distance from the uterus, since the fetus is mainly exposed to scattered radiation rather than direct radiation. In this case, shielding does not reduce fetal exposure to scattered radiation but provides psychological protection. When compared with shielding, the decreased scan length is the most effective means of reducing fetal absorbed doses [34-36]. In addition, when the shielding material is introduced into the scan region, the image optimization system of the CT scanner is forced to dramatically increase the radiation power of the tube, which ultimately increased the exposure dose to pregnant women and their fetuses [37].
CONCLUSION
Diagnostic radiology in pregnancy should be performed in accordance with radiological safety principles because of the likelihood of negative effects, and completely avoiding diagnostic techniques using ionizing radiation is a mistake.
Examinations using ionizing radiation may be necessary for various life-threatening conditions, and they are also preferred in the diagnosis of some diseases. Note that the risk of complications, arising from delayed diagnosis, many times exceeds the risk of negative effects from exposure to ionizing radiation.
These studies confirm that doses absorbed by the fetus during CT do not reach the threshold values. In chest CT, the doses absorbed by the fetus are insignificant and cannot lead to deterministic effects. More significant fetal radiation exposure occurs during abdominal and pelvic CT and whole-body scans; however, even in these studies, exceeding the permissible exposure threshold is unlikely if a single-phase examination is performed only once. Moreover, multiple abdominal or whole-body CT or multiphase CT with an intravenous contrast enhancement may lead to exceeding the permissible threshold for the absorbed dose of ionizing radiation. This information should be considered when referring a pregnant woman to CT in these areas. Other undesirable effects on fetal development when using contrast enhancement must be also considered.
ADDITIONAL INFORMATION
Funding source. This study was not supported by any external sources of funding.
Competing interests. The authors declare that they have no competing interests.
Authors’ contribution. All authors made a substantial contribution to the conception of the work, acquisition, analysis, interpretation of data for the work, drafting and revising the work, final approval of the version to be published and agree to be accountable for all aspects of the work. A.V. Vodovatov ― development of the study concept, systematization of data, peer review, and final editing of the systematic review; O.A. Golchenko — search for publications on the topic, analysis of literature data, design of tables, writing the text; I.A. Mashchenko ― development of the research concept, peer review and final editing of the systematic review; D.V. Alekseeva ― development of the study concept, analysis of the obtained data, final editing of the systematic review; L.A. Chipiga — data systematization, peer review, and final editing of the systematic review; I.V. Khutornoy — study design, statistical processing of the results, preparation of illustrations; P.V. Kozlova — search for publications on the topic, analysis of literature data, text editing; G.E. Trufanov ― development of the research concept, expert evaluation, approval of the final version of the article; P.S. Druzhinina — adaptation of the text of the article, processing of the research results; S.A. Ryzhov, setting research objectives, participating in the description of the discussion of the results obtained; I.V. Soldatov — participation in the discussion of the obtained results, expert evaluation, approval of the final version of the article.
About the authors
Aleksandr V. Vodovatov
Saint-Petersburg Research Institute of Radiation Hygiene after Professor P.V. Ramzaev
Email: vodovatoff@gmail.com
ORCID iD: 0000-0002-5191-7535
SPIN-code: 4560-8978
Cand. Sci. (Biol.)
Russian Federation, Saint PetersburgOlga A. Golchenko
City polyclinic № 19
Email: breakerxolyga@yandex.ru
ORCID iD: 0000-0003-4614-9241
Russian Federation, Saint Petersburg
Irina A. Mashchenko
Almazov National Medical Research Centre
Email: mashchenko_ia@almazovcentre.ru
ORCID iD: 0000-0002-4949-8829
SPIN-code: 5154-7080
MD, Cand. Sci. (Med.), Leading Researcher, Assistant Professor
Russian Federation, Saint PetersburgDarya V. Alekseeva
Almazov National Medical Research Centre
Email: darja-karpova@yandex.ru
ORCID iD: 0000-0001-9528-9377
SPIN-code: 6484-4327
Assistant Lecturer
Russian Federation, Saint PetersburgLarisa A. Chipiga
Saint-Petersburg Research Institute of Radiation Hygiene after Professor P.V. Ramzaev; Almazov National Medical Research Centre
Email: larisa.chipiga@gmail.com
ORCID iD: 0000-0001-9153-3061
SPIN-code: 3920-7798
Cand. Sci. (Engin.), Research Associate, Assistant Professor
Russian Federation, Saint Petersburg; Saint PetersburgIvan V. Khutornoy
Lomonosov Moscow State University
Email: mcdm.avk@gmail.com
ORCID iD: 0000-0002-5405-603X
SPIN-code: 8020-0222
Graduate Student
Russian Federation, MoscowPolina V. Kozlova
Almazov National Medical Research Centre
Email: apollinaria@bk.ru
ORCID iD: 0000-0002-3240-7038
SPIN-code: 3555-0410
Assistant Lecturer
Russian Federation, Saint PetersburgGennady E. Trufanov
Almazov National Medical Research Centre
Email: trufanovge@mail.ru
ORCID iD: 0000-0002-1611-5000
SPIN-code: 3139-3581
MD, Dr. Sci. (Med.)
Russian Federation, Saint PetersburgPolina S. Druzhinina
Saint-Petersburg Research Institute of Radiation Hygiene after Professor P.V. Ramzaev
Email: druzhininapauline@gmail.com
ORCID iD: 0000-0003-2921-067X
SPIN-code: 9003-3234
Junior Research Associate
Russian Federation, Saint PetersburgSergey A. Ryzhov
Research and Practice Center of Diagnostics and Telemedicine Technologies
Email: mosrg@mail.ru
ORCID iD: 0000-0002-0640-7368
SPIN-code: 6595-4011
Research Associate
Russian Federation, MoscowIlia V. Soldatov
Research and Practice Center of Diagnostics and Telemedicine Technologies
Author for correspondence.
Email: SoldatovIV2@zdrav.mos.ru
ORCID iD: 0000-0002-4867-0746
SPIN-code: 4065-6048
Russian Federation, Moscow
References
- Shtentsel RE, Semenova ES, Mashchenko IA, et al. The history of the formation and development of methods of radiation diagnostics in perinatology. Translational Med. 2021;8(3):29–36. (In Russ). doi: 10.18705/2311-4495-2021-8-3-29-36
- Sadro C, Bernstein MP, Kanal KM. Imaging of trauma. Part 2, Abdominal trauma and pregnancy: A radiologist’s guide to doing what is best for the mother and baby. Am J Roentgenol. 2012;199(6):1207–1219. doi: 10.2214/AJR.12.9091
- Wang PI, Chong ST, Kielar AZ, et al. Imaging of pregnant and lactating patients: Part 1, evidence-based review and recommendations. Am J Roentgenol. 2012;198(4):778–784. doi: 10.2214/AJR.11.7405
- Committee Opinion No. 723: Guidelines for diagnostic imaging during pregnancy and lactation. Obstet Gynecol. 2017;130(4):210–216. doi: 10.1097/AOG.0000000000002355
- ICRP. Recommendations International Commission on Radiation Protection 2007. Publication ICRP No. 103. Transl. from English. Ed. by M.F. Kiselev and N.K. Shandala. Moscow: Alana; 2009. 312 р.
- ACR-SPR practice parameter for imaging pregnant or potentially pregnant adolescents and women with ionizing radiation. 2018. 23 p. Available from: https://www.acr.org/-/media/acr/files/practice-parameters/pregnant-pts.pdf. Accessed: 17.05.2023.
- Frush D. The cumulative radiation dose paradigm in pediatric imaging. Br J Radiol. 2021;94(1126):20210478. doi: 10.1259/bjr.20210478
- Vodovatov AV, Chipiga LA, Piven PA, et al. Assessment of the absorbed doses in the fetus from the computed tomography of the chest for the pregnant women. Radiatsionnaya Gygiena. 2021;14(3):126–135. (In Russ). doi: 10.21514/1998-426X-2021-14-3-126-135
- Liu H, Liu F, Li J, et al. Clinical and CT imaging features of the COVID-19 pneumonia: Focus on pregnant women and children. J Infect. 2020;80(5):7–13. doi: 10.1016/j.jinf.2020.03.007
- Dehan L, Lin L, Xin W, et al. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: A preliminary analysis. Am J Roentgenol. 2020;215(1):127–132. doi: 10.2214/AJR.20.23072
- Garcia EM, Camacho MA, Karolyi DR, et al.; Expert Panel on Gastrointestinal Imaging. ACR appropriateness criteria right lower quadrant pain-suspected appendicitis. Am J Roentgenol. 2018;15(11):373–387. doi: 10.1016/j.jacr.2018.09.033
- Sazhin AV, Kirienko AI, Kurtser MA, et al. Acute appendicitis during pregnancy (in Russian only). Pirogov Russian Journal of Surgery. 2019;(1):70–77. (In Russ).
- Gu J, Bednarz B, Caracappa PF, Xu XG. The development, validation and application of a multi-detector CT (MDCT) scanner model for assessing organ doses to the pregnant patient and the fetus using Monte Carlo simulations. Phys Med Biol. 2009;54(9):2699–2717. doi: 10.1088/0031-9155/54/9/007
- Kelaranta A, Mäkelä T, Kaasalainen T, Kortesniemi M. Fetal radiation dose in three common CT examinations during pregnancy: Monte Carlo study. Phys Med. 2017;(43):199–206. doi: 10.1016/j.ejmp.2017.09.120
- Angel E, Wellnitz CV, Goodsitt MM, et al. Radiation dose to the fetus for pregnant patients undergoing multidetector CT imaging: Monte Carlo simulations estimating fetal dose for a range of gestational age and patient size. Radiology. 2008;249(1):220–227. doi: 10.1148/radiol.2491071665
- Goldberg-Stein S, Liu B, Hahn PF, Lee SI. Body CT during pregnancy: Utilization trends, examination indications, and fetal radiation doses. Am J Roentgenol. 2011;196(1):146–151. doi: 10.2214/AJR.10.4271
- Vandecaveye V, Amant F, Lecouvet F, et al. Imaging modalities in pregnant cancer patients. Int J Gynecol Cancer. 2021;31(3):423–431. doi: 10.1136/ijgc-2020-001779
- Kwan ML, Miglioretti DL, Marlow EC, et al.; Radiation-Induced Cancers Study Team. Trends in medical imaging during pregnancy in the United States and Ontario, Canada, 1996 to 2016. JAMA Network Open. 2019(7):197–249. doi: 10.1001/jamanetworkopen.2019.7249
- Prokop M, Galanski M. Spiral and multilayered computed tomography. Moscow; 2011. 440 р. (In Russ).
- Arablinskiy AV, Magdebura YA. CT in the diagnosis of nontraumatic acute abdomen. REJR. 2018;8(2):58–71. (In Russ). doi: 10.21569/2222-7415-2018-8-2-58-71
- Kirsch J, Brown RK, Henry TS, et al.; Expert Panels on Cardiac and Thoracic Imaging. ACR appropriateness criteria acute chest pain-suspected pulmonary embolism. J Am Coll Radiol. 2017;14(5):2–12. doi: 10.1016/j.jacr.2017.02.027
- Shyu JY, Khurana B, Soto JA, et al. Expert Panel on Major Trauma Imaging. ACR appropriateness criteria major blunt trauma. J Am Coll Radiol. 2020;17(5):160–174. doi: 10.1016/j.jacr.2020.01.024
- Panchenko EP, Balahonova TV, Danilov NM, et al. Diagnosis and management of pulmonary embolism Eurasian Association of Cardiology (EAC) clinical practice guidelines (2021). Eurasian Heart J. 2021;(1):44–77. (In Russ). doi: 10.381092225-1685-2021-1-44-77
- Ria F, D’Ercole L, Origgi D, et al.; Association of Medical Physics Task Group. Statement of the Italian Association of Medical Physics (AIFM) task group on radiation dose monitoring systems. Insights Imaging. 2022;13(1):23. doi: 10.1186/s13244-022-01155-1
- Sensakovic WF, Royall I, Hough M, et al. Fetal dosimetry at CT: A primer. Radiographics. 2020;40(4):1061–1070. doi: 10.1148/rg.2020190166
- Jaffe TA, Yoshizumi TT, Toncheva GI, et al. Early first-trimester fetal radiation dose estimation in 16-MDCT without and with automated tube current modulation. Am J Roentgenol. 2008;190(4):860–864. doi: 10.2214/AJR.07.2925
- Huda W, Randazzo W, Tipnis S, et al. Embryo dose estimates in body CT. Am J Roentgenol. 2010;194(4):874–880. doi: 10.2214/AJR.09.4032
- Damilakis J, Perisinakis K, Tzedakis A, et al. Radiation dose to the conceptus from multidetector CT during early gestation: A method that allows for variations in maternal body size and conceptus position. Radiology. 2010;257(2):483–489. doi: 10.1148/radiol.10092397
- Lazarus E, Debenedectis C, North D, et al. Utilization of imaging in pregnant patients: 10-year review of 5270 examinations in 3285 patients 1997–2006. Radiology. 2009;251(2):517–524. doi: 10.1148/radiol.2512080736
- Lazarus E, Mayo-Smith WW, Mainiero MB, Spencer PK. CT in the evaluation of nontraumatic abdominal pain in pregnant women. Radiology. 2007;244(3):784–790. doi: 10.1148/radiol.2443061634
- Goldberg-Stein SA, Liu B, Hahn PF, Lee SI. Radiation dose management: Part 2, estimating fetal radiation risk from CT during pregnancy. Am J Roentgenol. 2012;198(4):352–356. doi: 10.2214/AJR.11.7458
- Litmanovich D, Boiselle PM, Bankier AA, et al. Dose reduction in computed tomographic angiography of pregnant patients with suspected acute pulmonary embolism. J Comput Assist Tomogr. 2009;33(6):961–966. doi: 10.1097/RCT.0b013e318198cd18
- Begano D, Söderberg M, Bolejko A. To use or not use patient shielding on pregnant women undergoing CT pulmonary angiography: A phantom study. Radiation Protection Dosimetry. 2020;189(4):458–465.
- Ryckx N, Sans-Merce M, Schmidt S, et al. The use of out-of-plane high Z patient shielding for fetal dose reduction in computed tomography: Literature review and comparison with Monte-Carlo calculations of an alternative optimisation technique. Phys Med. 2018;(48):156–161. doi: 10.1016/j.ejmp.2018.03.017
- Tack D, Kalra MK, Gevenois PA. Radiation dose from multidetector CT (2nd ed.). Springer; 2012. doi: 10.1007/978-3-642-24535-0
- Doshi SK, Negus IS, Oduko JM. Fetal radiation dose from CT pulmonary angiography in late pregnancy: A phantom study. Br J Radiol. 2008;81(968):653–658. doi: 10.1259/bjr/22775594
- Gilet AG, Dunkin JM, Fernandez TJ, et al. Fetal radiation dose during gestation estimated on an anthropomorphic phantom for three generations of CT scanners. Am J Roentgenol. 2011;196(5):1133–1137. doi: 10.2214/AJR.10.4497
Supplementary files