Volume 6, Nº 2 (2025)
- Ano: 2025
- ##issue.datePublished##: 08.07.2025
- Artigos: 12
- URL: https://jdigitaldiagnostics.com/DD/issue/view/9912
- DOI: https://doi.org/10.17816/DD.62
Edição completa
Original Study Articles
Possibilities of Dixon sequences in magnetic resonance imaging for fat fraction quantification: a phantom study
Resumo
BACKGROUND: The accuracy of quantitative parameters obtained using magnetic resonance imaging is of scientific and practical interest. Monitoring of scan parameters and standardization of commonly used approaches to assess fat fraction remain challenging in radiology.
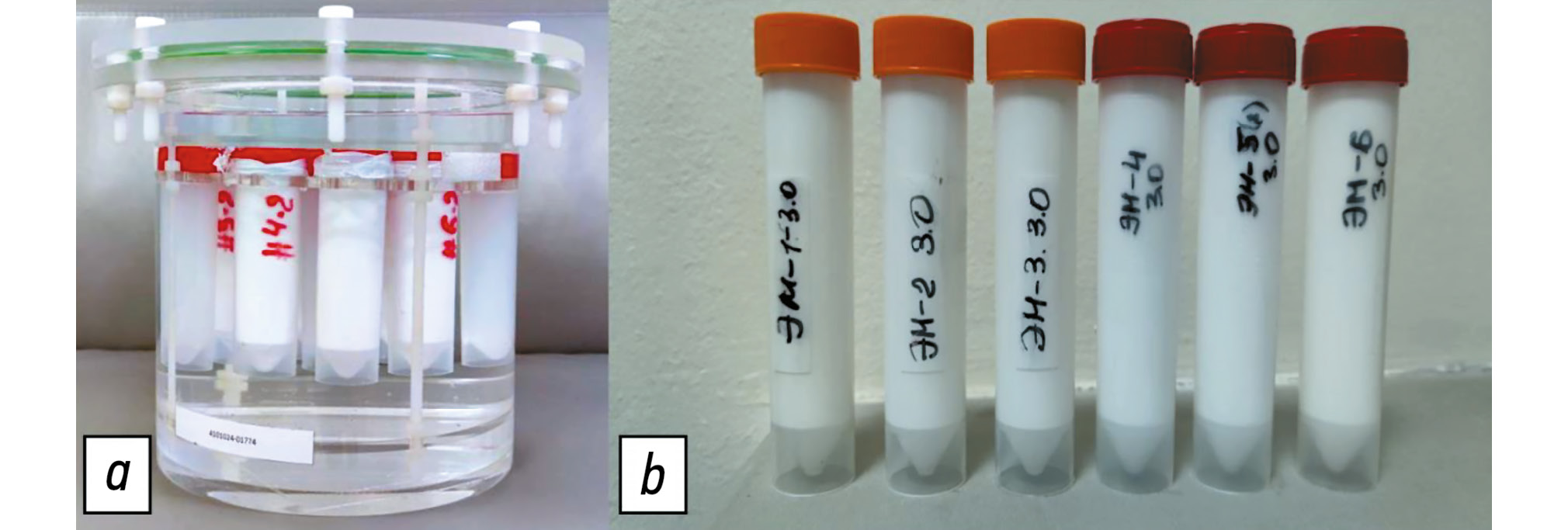
AIM: This study aimed to evaluate the possibility of fat fraction quantification using standard Dixon pulse sequences through phantom modeling.
METHODS: This multicenter, cross-sectional, nonblinded experimental study used direct oil-in-water emulsions to model substances with varying fat concentrations. Test tubes containing these emulsions were placed in a cylindrical phantom. The emulsions were prepared with mixtures of vegetable oils, with fat fraction values of 10%–60%. Several tests were conducted using scanners from different manufacturers and with varying magnetic field strengths: Optima MR450w, 1.5 T; MAGNETOM Skyra, 3 T; Ingenia, 1.5 T; and Ingenia Achieva dStream, 3.0 T at different medical centers. Fat fraction was obtained using standard formulas based on signal intensity measurements. A regression analysis was conducted to assess the linear relationship between the measured and predefined fat fraction concentrations and an F-test to evaluate variability.
RESULTS: Phantom modeling was employed to determine the performance of Dixon pulse sequences across different magnetic resonance imaging scanners for quantitative fat fraction estimation using relevant formulas. In assessing the accuracy of fat fraction quantification, a weak linear correlation was found between the obtained values and predefined fat fraction concentrations. Additionally, significant deviations >5% were observed for certain scanners. Reproducibility analysis demonstrated variability in fat fraction concentration across different scanner models and within the same model.
CONCLUSION: Obtained results confirm that fat fraction quantification using Dixon pulse sequences and relevant formulas should be performed only after preliminary phantom scanning. The use of a phantom ensures adequate quality control and calibration of the magnetic resonance imaging scanner, making accurate quantitative fat measurement more reliable and widely accessible.
 191-202
191-202


Comparison of non-contrast magnetic resonance perfusion and phase-contrast angiography for the quantitative assessment of cerebral blood flow: a prospective cross-sectional study
Resumo
BACKGROUND: The validation of quantitative cerebral blood flow assessment using non-contrast magnetic resonance imaging remains unresolved. The optimal approach involves applying a method based on a different physiological model to enhance the reliability of the obtained data.
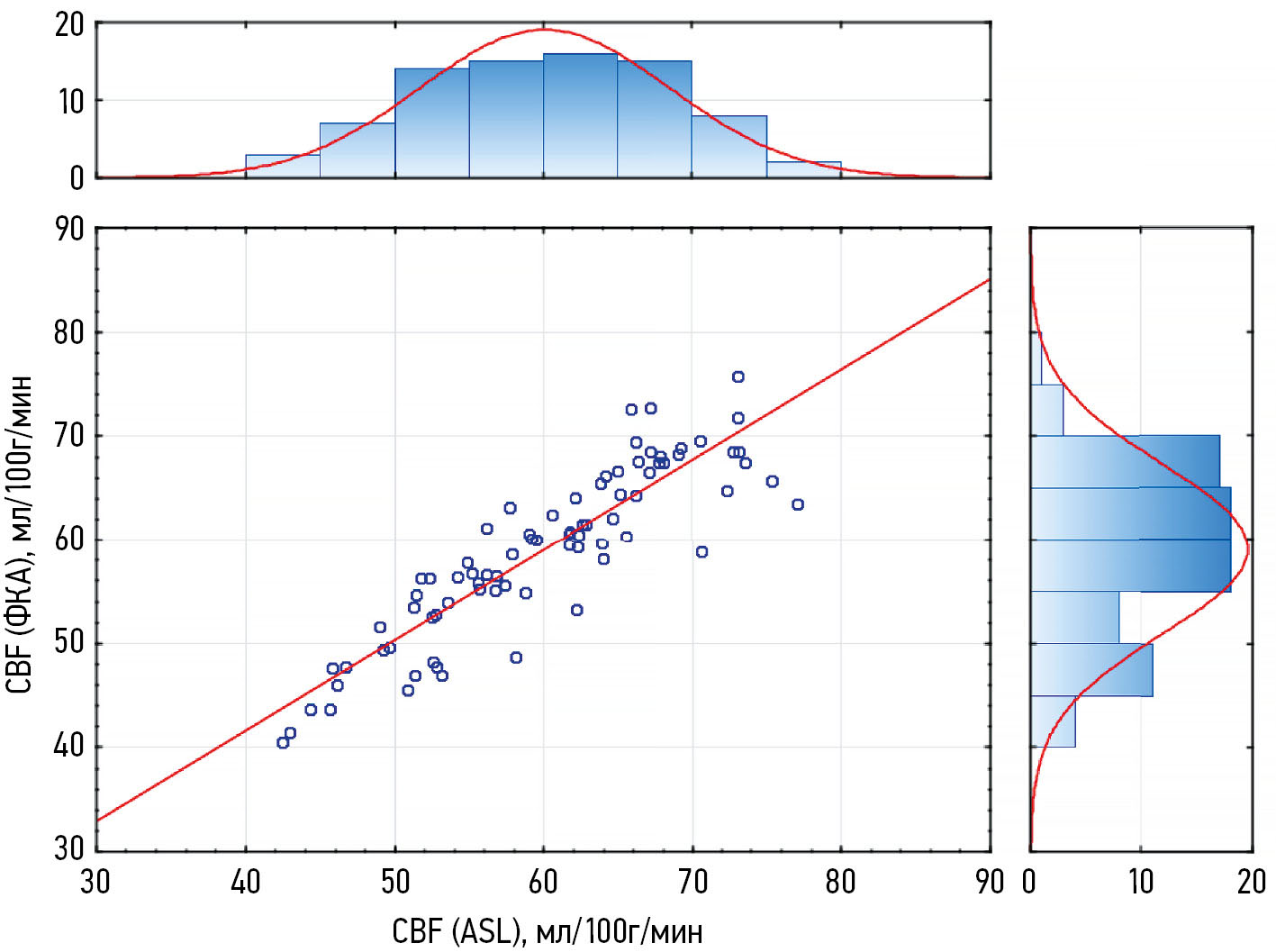
AIM: To verify the results of quantitative cerebral tissue blood flow assessment using non-contrast MRI against quantitative 2D phase-contrast angiography in healthy adults.
METHODS: The prospective study enrolled healthy adults (aged 18–75 years). Cerebral perfusion was assessed using non-contrast magnetic resonance imaging, while macrovascular blood flow was measured in the vertebral and internal carotid arteries using quantitative 2D phase-contrast angiography. Brain volume and relative mass were evaluated based on T1-weighted image segmentation. Macrovascular blood flow values were converted into tissue perfusion metrics through mathematical adjustment accounting for brain mass.
RESULTS: In the study 80 adults were examined using both methods. Non-contrast magnetic resonance imaging revealed mean perfusion values of 17.88 ± 2.39 mL/100g/min in white matter and 42.06 ± 7.13 mL/100g/min in gray matter, with total cerebral perfusion at 59.63 ± 8.56 mL/100g/min. Total cerebral perfusion calculated from phase-contrast angiography and arterial blood flow velocity was 58.96 ± 8.16 mL/s. A strong positive correlation was found between total cerebral perfusion values derived from non-contrast magnetic-resonance and phase-contrast angiography (r = 0.892; p < 0.001).
CONCLUSION: A strong positive correlation was demonstrated between cerebral perfusion values obtained via non-contrast magnetic resonance imaging and phase-contrast angiography, despite their reliance on distinct physiological models.
 203-213
203-213


Diagnosis of intracranial hemorrhages based on brain computed tomography with artificial intelligence
Resumo
BACKGROUND: Intracranial hemorrhages are associated with high mortality and risk of disability, requiring prompt and accurate diagnosis, particularly within the first 24 hours. The use of artificial intelligence technologies in analyzing brain computed tomography scans can shorten diagnostic time and improve diagnostic quality. The relevance of this study is emphasized by the limited number of certified artificial intelligence services for detecting intracranial hemorrhages in Russia and lacking data on their long-term effectiveness, highlighting the need for multicenter monitoring to assess the stability and accuracy of such systems in clinical practice.
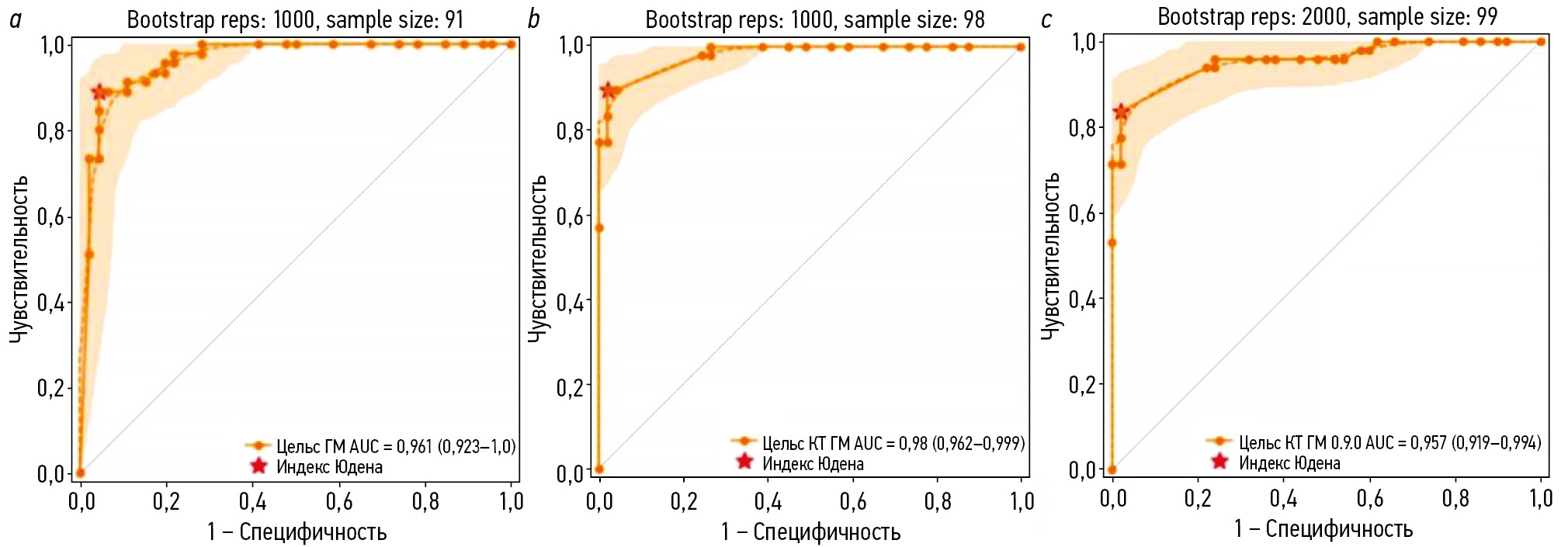
AIM: The study aimed to assess the diagnostic accuracy and stability of an artificial intelligence service in detecting intracranial hemorrhages on non-contrast brain computed tomography scans in a multicenter clinical monitoring setting for 18 months.
METHODS: Anonymized brain computed tomography scans were used. The artificial intelligence service underwent a three-phase evaluation to evaluate its diagnostic accuracy and clinical performance using limited datasets. Two radiologists specializing in neuroimaging examined 80 brain computed tomography scans each month for 18 months, which had been preprocessed by the artificial intelligence service and randomly selected from the clinical workflow. The results were analyzed using ROC analysis with sensitivity, specificity, accuracy, and area under the curve.
RESULTS: During clinical monitoring, 1200 brain computed tomography scans were analyzed, with signs of intracranial hemorrhage detected in 48.3% of the scans. Based on the binary classification of intracranial hemorrhage presence or absence performed by the artificial intelligence service, the following diagnostic metrics were obtained: sensitivity, 97.4% (95.8–98.5); specificity, 75.4% (71.8–78.7); accuracy, 86.0% (83.9–87.9); and area under the curve, 94% (92.6–95.3). Eventually, a significant moderate positive correlation was observed in most diagnostic metrics and the time variable, except for sensitivity, which was affected by an update to the service version. However, full concordance between artificial intelligence-based markings and radiologist conclusions was noted in 28.5% of cases of identified intracranial hemorrhage, whereas discrepancies were found in 71.5%. The refined diagnostic metrics for cases with complete agreement with the radiologists’ report were as follows: sensitivity, 26.6%; specificity, 73.8%; accuracy, 50.1%; and area under the curve, 49.6%.
CONCLUSION: The current configuration of the artificial intelligence service allows ruling out intracranial hemorrhage with very high probability, which may be useful in the initial triaging of patients in emergency settings. However, low values of refined metrics indicate considerable discrepancies between radiologist reports and service-generated results regarding the interpretation of pathological findings.
 214-228
214-228


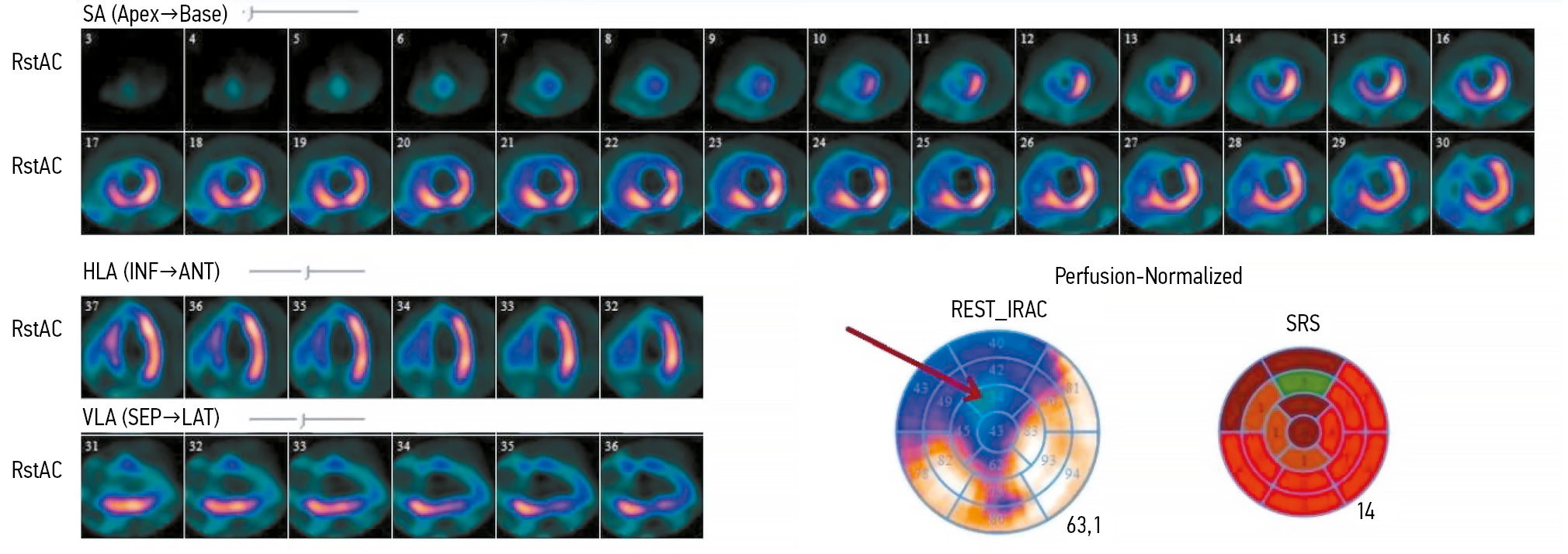
Optimization of left ventricular lead implantation based on combined myocardial perfusion scintigraphy and computed tomography data
Resumo
BACKGROUND: Successful cardiac resynchronization therapy in patients with chronic heart failure critically depends on the selection of the optimal implantation site for the left ventricular lead. A hybrid imaging approach combining cardiac venous computed tomography and myocardial perfusion scintigraphy may assist in identifying the target vein and improve procedural efficacy.
AIM: The work aimed to evaluate the feasibility of a multimodal imaging approach for optimizing left ventricular lead implantation in cardiac resynchronization therapy.
METHODS: It was a prospective, observational, single-center, non-randomized controlled study. Patients with chronic heart failure and indications for cardiac resynchronization therapy in accordance with current guidelines were enrolled. Prior to the procedure, the patients underwent computed tomography of the cardiac veins to visualize venous anatomy and myocardial perfusion scintigraphy to assess the extent of left ventricular perfusion impairment. The optimal site for left ventricular lead placement was identified using a three-dimensional reconstruction of the coronary sinus fused with myocardial perfusion scintigraphy data. To assess the effectiveness of the hybrid approach, a reference group was formed, in which cardiac resynchronization implantation was performed using the standard method, without preprocedural evaluation of coronary venous anatomy or myocardial scarring. Six months after cardiac resynchronization therapy, all patients underwent echocardiography to evaluate treatment effectiveness. Echocardiographic response was defined as a reduction in left ventricular end-systolic volume by ≥15% and/or an increase in ejection fraction by ≥5%.
RESULTS: The imaging group consisted of 40 patients with chronic heart failure, whereas the reference group included 30 patients with the same diagnosis. Six months after cardiac resynchronization therapy, a positive treatment response was observed in 33 patients (82%) in the imaging group, significantly higher than in the reference group (17 patients, 57%), p = 0.031. In the imaging group, the reduction in left ventricular end-systolic volume was statistically significant compared with the reference group and amounted to −52 [−71; −22.5] mL versus −21 [−64; −1] mL, respectively (p = 0.039). The increase in left ventricular ejection fraction was 7.5 [4.5; 15]% in the imaging group and 4.5 [0; 13]% in the reference group, with no statistically significant difference (p = 0.082).
CONCLUSION: The use of cardiovascular imaging methods, including cardiac venous computed tomography and myocardial perfusion scintigraphy, was associated with an increased proportion of responders to cardiac resynchronization therapy.
 229-238
229-238


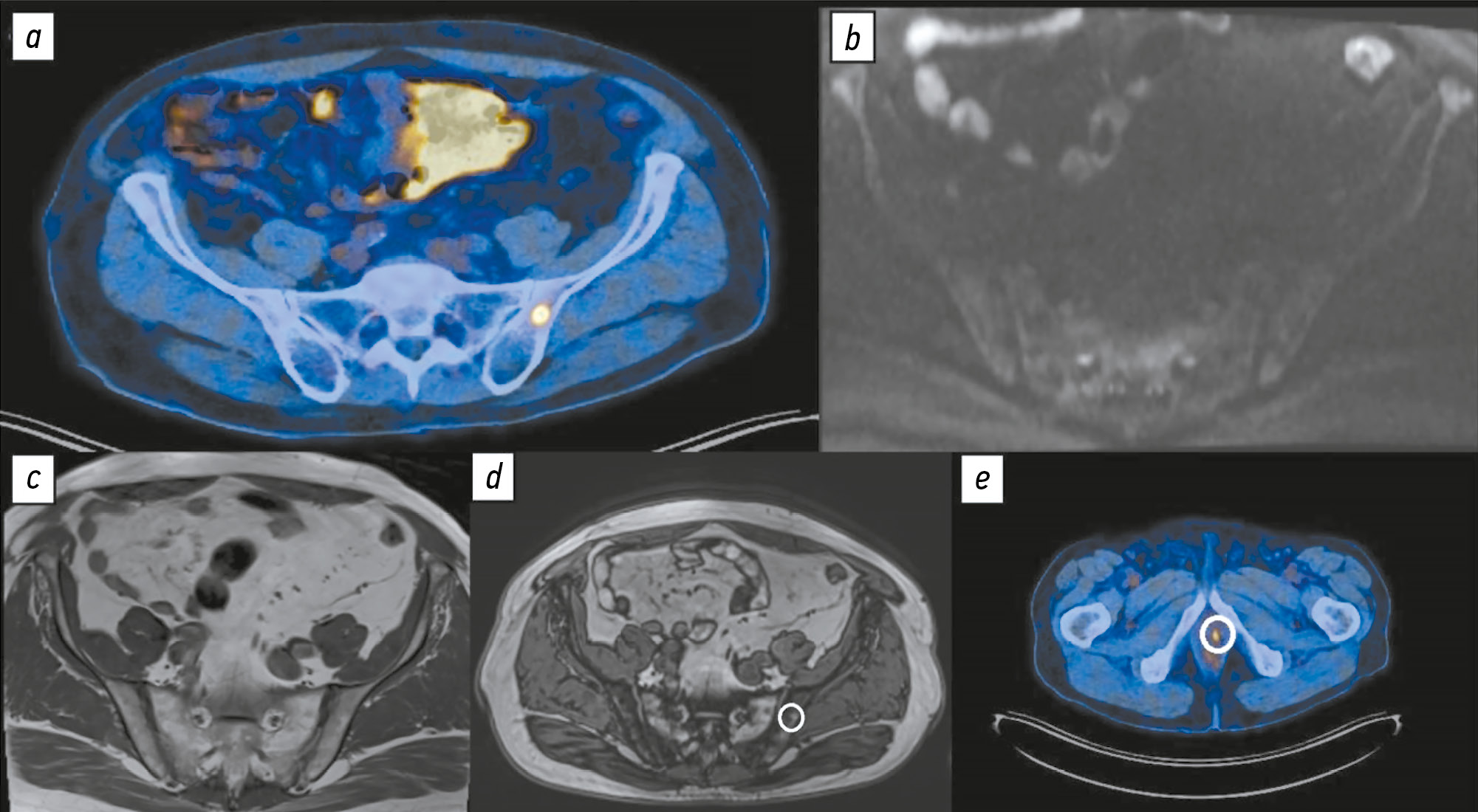
Comparison of the diagnostic accuracy of whole-body diffusion-weighted imaging and 18F-prostate-specific membrane antigen-1007 positron emission tomography combined with computed tomography for detecting bone metastases in prostate cancer
Resumo
BACKGROUND: The increasing availability of 18F-prostate-specific membrane antigen-1007 (18F-PSMA-1007) for prostate cancer staging highlighted its advantages, particularly its higher spatial resolution compared to analogs. Moreover, accumulating scientific data indicate an increase in false-positive findings, predominantly in bones, which may lead to unwarranted upstaging of the disease. Diffusion-weighted imaging may be used for the early detection of bone metastases.
AIM: This study aimed to assess and compare the diagnostic accuracy of whole-body 18F-PSMA-1007 positron emission tomography combined with computed tomography and whole-body and pelvic bone diffusion-weighted imaging in patients with prostate cancer.
METHODS: A retrospective single-center selective study was conducted. The imaging results of 119 patients with prostate cancer were divided into two groups: group 1 comprised 40 pairs of 18F-PSMA-1007 positron emission tomography combined with computed tomography and whole-body diffusion-weighted magnetic resonance imaging scans, and group 2 included 79 pairs of similar studies, with magnetic resonance imaging performed only for the pelvic bones. The diagnostic studies were performed at an inter-study interval ≤14 days. The metastatic bone lesions detected in different anatomical regions was counted using data from 18F-PSMA-1007 positron emission tomography combined with computed tomography and magnetic resonance imaging. Lesions were considered true positives if confirmed by additional magnetic resonance imaging pulse sequences and/or follow-up observation.
RESULTS: Whole-body diffusion-weighted imaging demonstrated higher specificity (58.1%) for detecting bone metastases than 18F-PSMA-1007 positron emission tomography combined with computed tomography (51.06%). However, its sensitivity was lower: 93.22% versus 97.55%.
CONCLUSION: Despite its advantages, 18F-PSMA-1007 positron emission tomography combined with computed tomography shows a high rate of false-positive bone findings. These are most commonly noted in the ribs, vertebrae, and pelvic bones. Suspicious bone lesions should be further evaluated to avoid unjustified disease upstaging. Thus, whole-body magnetic resonance imaging with diffusion-weighted sequences and selective fat signal suppression can be used.
 239-250
239-250


Systematic reviews
Use of artificial intelligence technologies in laboratory medicine, their effectiveness and application scenarios: a systematic review
Resumo
BACKGROUND: With the increasing volume of data, laboratory medicine requires automation and standardization of routine processes to reduce workload on healthcare professionals and clear their time for more specialized tasks. Machine learning models and artificial neural networks support image recognition and analysis of large data sets, which allows their integration into laboratory workflows to solve routine tasks.
AIM: This study aimed to analyze global scientific publications on the application of artificial intelligence technologies in laboratory medicine and their potential to address current challenges and identify barriers in their integration into laboratory workflows.
METHODS: A search for publications was conducted using PubMed, manufacturer websites offering ready-to-use laboratory solutions, and reference lists from other reviews. The Mendeley software was utilized for bibliographic data management. The search covered the time interval 2019–2024. Obtained data included bibliometric indicators, research areas, key methodological characteristics, diagnostic effectiveness values for artificial intelligence systems and healthcare professionals, the number and experience of involved healthcare professionals, and validated outcomes of artificial intelligence implementation. The study quality was assessed using a modified QUADAS-CAD checklist.
RESULTS: Twenty-three publications presenting studies at the pre-analytical (n = 1), analytical (n = 19), and post-analytical (n = 3) stages of laboratory analysis were included. Most studies focused on cytology and microbiology, accounting for 48% and 35% of the studies, respectively. Artificial intelligence demonstrated high effectiveness in solving tasks across all stages of the laboratory process. Moreover, its diagnostic accuracy was comparable to that of healthcare professionals; however, decision-making speed was higher. All studies demonstrated a risk of systematic bias, which was associated with unbalanced samples, lacking external data validation, and incomplete description of datasets and analytical methods.
CONCLUSION: Artificial intelligence demonstrates high potential in diagnostic accuracy and processing speed, making it a promising tool to be integrated into laboratory practice and automation of routine processes. However, to achieve this, research methodologies for artificial intelligence should be standardized to reduce the risk of systematic bias, establish reference values for laboratories to ensure the reproducibility and generalizability of results, raise awareness among healthcare professionals and patients on how artificial intelligence works to overcome prejudices, and develop reliable mechanisms for protecting personal data when using artificial intelligence.
 251-267
251-267


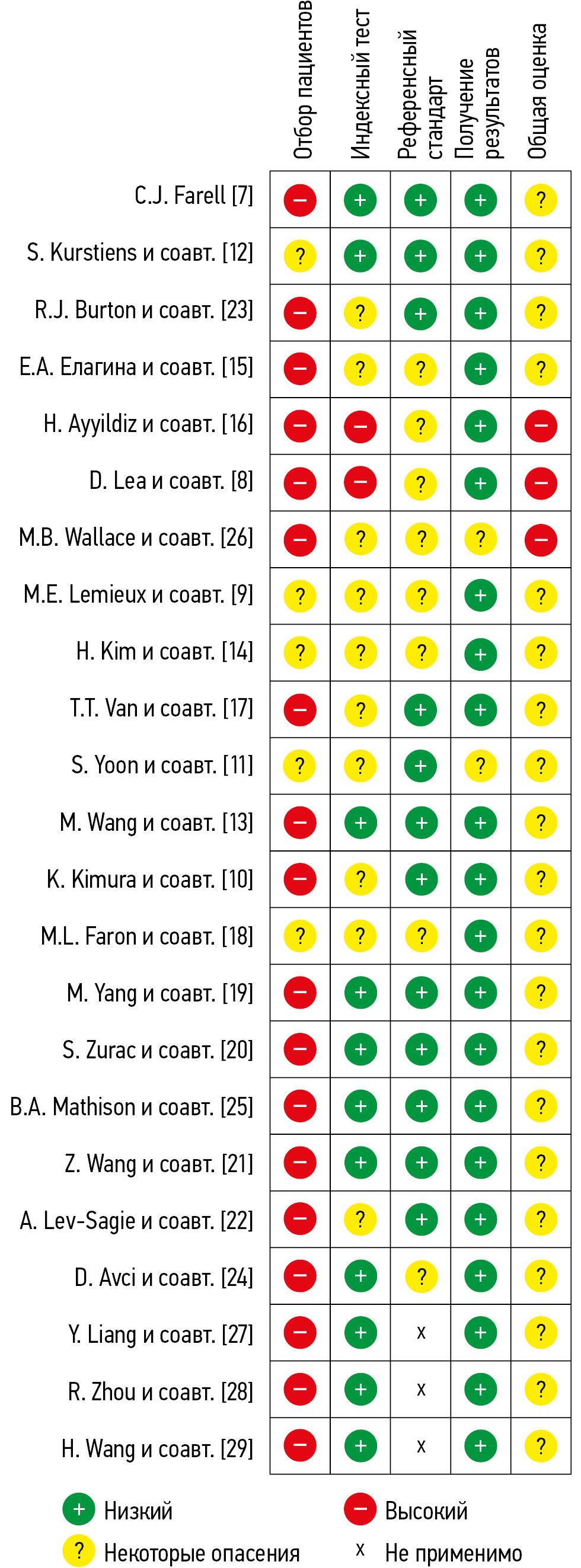
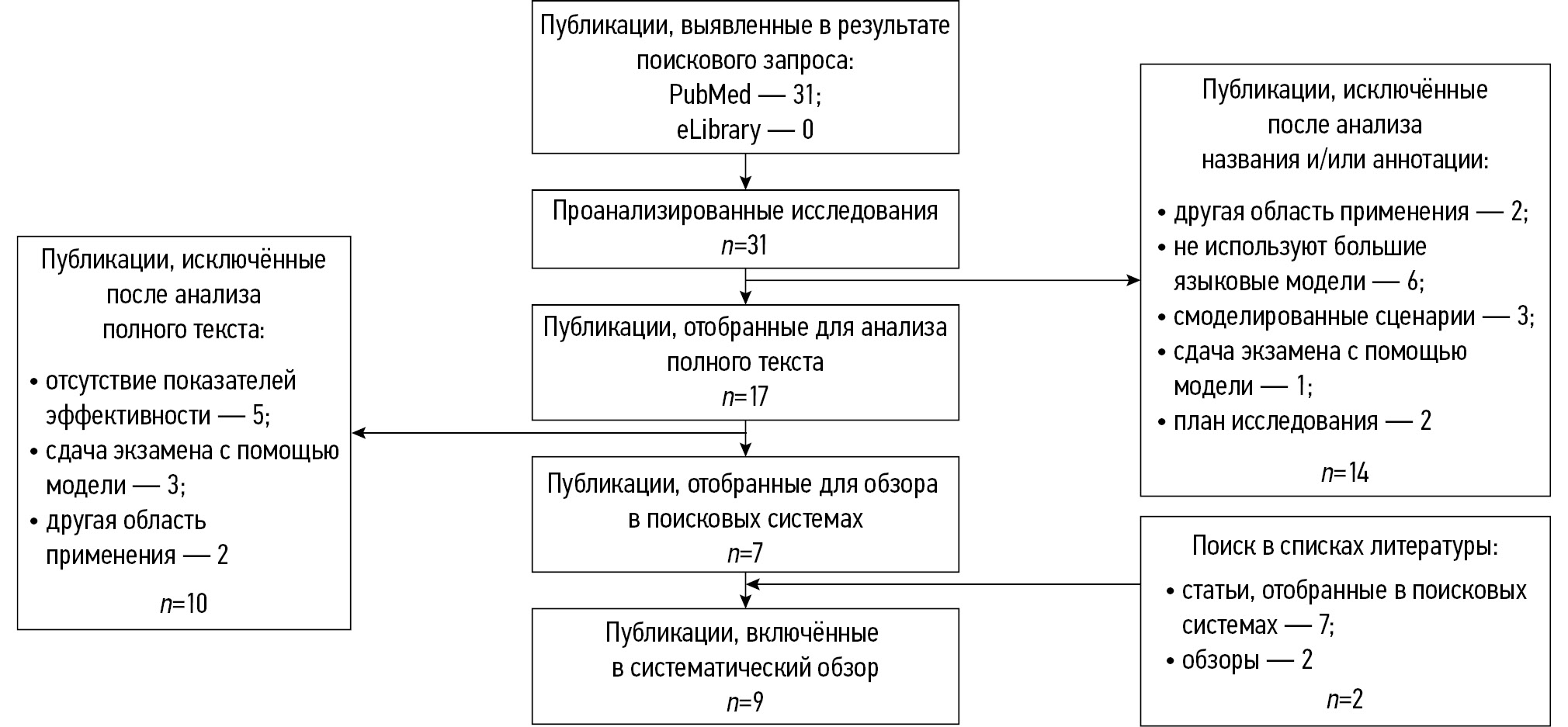
Application of large language models in radiological diagnostics: a scoping review
Resumo
BACKGROUND: Modern large language models show potential for application in radiological diagnostics across a wide range of routine tasks.
AIM: The work aimed to conduct a scoping review of the application of large language models in radiological diagnostics by analyzing possible use-case scenarios and assessing the methodological quality of relevant studies.
METHODS: Two search strategies were employed: a primary search (PubMed and eLibrary) targeting full-text publications with well-developed methodology, and a supplementary search (PubMed) aimed at broader coverage of large language model use cases in radiological diagnostics during 2023–2025. Extracted data included bibliometric characteristics, study objectives, use-case scenarios of large language models, nosological profiles, key methodological parameters, and both quantitative and qualitative indicators of diagnostic performance—for both the models and the specialists involved, including their number and experience. The quality was assessed using the modified QUADAS-CAD questionnaire.
RESULTS: The primary search yielded 9 studies for analysis; the supplementary search yielded 216. A total of 9 major use-case scenarios for large language models in radiology were identified. The most common among them was the rephrasing of radiology reports in order to improve their accessibility for patient understanding. Models predominantly used were GPT-4 and BERT, along with GPT-3.5, Llama 2, Med42, GPT-4V, and Gemini Pro. The large language model GPT-4 demonstrated high diagnostic accuracy in identifying brain tumors (73.0%), myocarditis (83.0%), and in making decisions on invasive procedures for acute coronary syndrome (86.0%). In turn, it demonstrated low diagnostic accuracy for nervous system disorders of various etiologies (50.0%) and for musculoskeletal diseases (43.0%). The BERT model exhibited high diagnostic accuracy in detecting pulmonary nodules (99.0%) and signs of intracranial hemorrhage (sensitivity and specificity: 97.0% and 90.0%, respectively), as well as in report classification (accuracy: 84.3%).
Most articles (88.9%) carried a high risk of bias. The main reasons for this included small and imbalanced sample sizes, overlap between training and test datasets, and insufficiently precise preparation and description of reference standards.
CONCLUSION: The diagnostic performance of large language models varies significantly across articles. Their clinical implementation requires standardized, methodologically robust research, including larger and more balanced samples, optimization of the structure and volume of datasets, separation of training and testing samples, thorough preparation and description of reference standards, as well as the accumulation of empirical data for specific radiological tasks.
 268-285
268-285


Reviews
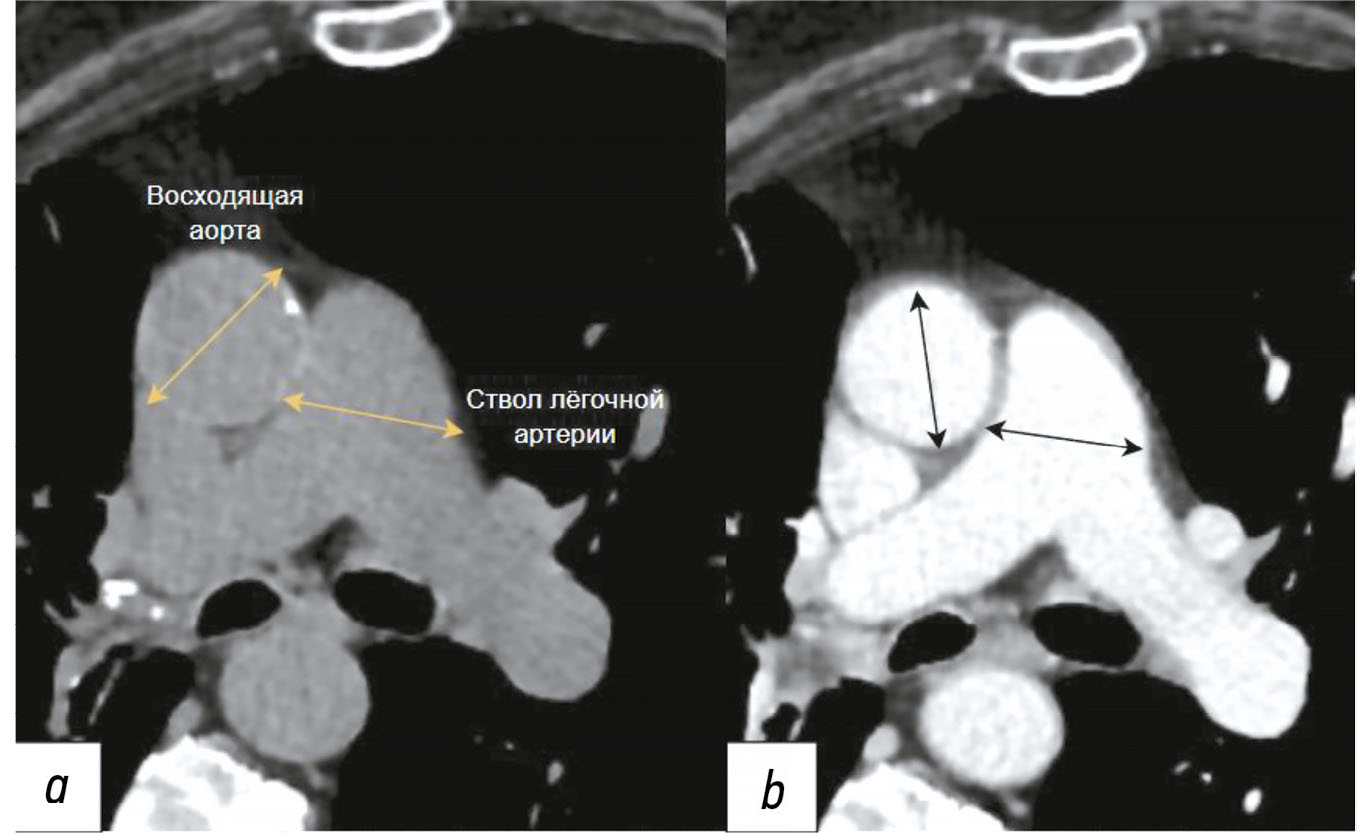
Diagnosis of thoracic aortic aneurysms and pathological pulmonary trunk dilation using chest computed tomography and artificial intelligence: modern approaches and prospects (a review)
Resumo
Early diagnosis of thoracic aortic aneurysms and pathological pulmonary trunk dilation is crucial to prevent severe complications, including vascular wall rupture and acute right ventricular failure, and reduce cardiovascular mortality. This review examines contemporary imaging approaches for these conditions, focusing on computed tomography as the gold standard modality. Emphasis was placed on the implementation of artificial intelligence technologies, which enable automatic segmentation of vascular structures, measurement of their diameter, and opportunistic screening, allowing early detection of asymptomatic conditions without additional diagnostic procedures, thereby reducing radiologist workload and improving medical care quality. The study comprehensively analyzed the Moscow Experiment, wherein the application of artificial intelligence in medical image analysis showed high sensitivity, reproducibility, and reduced reporting time. Despite these significant advantages, the need for expert supervision of artificial intelligence-generated results to ensure diagnostic accuracy and reliability is emphasized. Moreover, the review highlights the importance of adapting algorithms to different scanning protocols and population-specific features. Additionally, the importance of interdisciplinary collaboration among cardiologists, radiologists, data scientists, and software developers for the effective integration into routine clinical practice is pointed out. Therefore, the review outlines the potential of artificial intelligence technologies to enhance diagnostic quality and underscores the need for further clinical research and standardization of methods for successful integration into daily practice.
 286-301
286-301


Determination of bone age based on hand radiography: from classical methods to artificial intelligence (a review)
Resumo
Bone age assessment methods are crucial in diagnosing diseases associated with growth and developmental disorders, especially in pediatric practice. These methods have advantages and limitations, and their accuracy may vary depending on population-specific characteristics.
This article outlines the current state and potential of bone age assessment methods, including solutions based on artificial intelligence technologies.
Scientific data on bone age assessment over the past 10 years were explored using PubMed and eLibrary. Earlier publications that serve as reference points in the development of bone age assessment methodology—such as atlases, guidelines, and relevant studies—were included. Publications addressing the prevalence and practical use of various bone age assessment techniques, including radiography, ultrasound, computed tomography, magnetic resonance imaging, and artificial intelligence, were prioritized. The search was performed using the following keywords: bone age, bone age assessment, radiography, artificial intelligence, deep learning, growth development, AI, костный возраст (bone age), рентгенография (radiography), and искусственный интеллект (artificial intelligence).
This review demonstrates the wide range of existing bone age assessment methods and emphasizes the importance of new technologies such as artificial intelligence in improving diagnostic accuracy. Modern automated techniques show potential for optimizing diagnostic workflows in pediatric care and contribute to the early detection of growth and developmental disorders.
 302-316
302-316


Role of artificial intelligence and novel visualization techniques in the early diagnosis of pancreatic cancer: a review
Resumo
Pancreatic ductal adenocarcinoma is the most common pancreatic cancer. It is characterized by a progressive course or distant metastases in 80%–85% of cases. Despite advances in understanding of pancreatic ductal adenocarcinoma, the disease is consistently linked to poor prognosis due to late diagnosis and limited treatment options in advanced stages. Recently, image processing using artificial intelligence has been introduced for pancreatic ductal adenocarcinoma diagnosis and demonstrated promising results. This review summarizes current scientific data, evaluates the role of artificial intelligence in imaging and early detection of pancreatic ductal adenocarcinoma, and identifies issues that warrant further investigation. The search for publications was conducted using PubMed, Google Scholar, and eLibrary. The following Russian and English search keywords were used: ранняя диагностика рака поджелудочной железы (early diagnosis of pancreatic cancer), искусственный интеллект (artificial intelligence), протоковая аденокарцинома поджелудочной железы (pancreatic ductal adenocarcinoma), медицинская визуализация (medical visualization), наночастицы (nanoparticles), pancreatic cancer, artificial intelligence, early diagnosis pancreatic ductal adenocarcinoma, and pancreatic cancer imaging. Significant progress in early detection of pancreatic ductal adenocarcinoma using artificial intelligence technologies was observed. Current approaches include pre-imaging risk stratification and increased data volume by analyzing electronic medical records. Despite substantial achievements, the clinical implementation of artificial intelligence technologies remains challenging. The use of artificial intelligence along with biomarkers is a promising direction and may enhance theranostics of various malignancies, including pancreatic ductal adenocarcinoma.
 317-330
317-330


Radiomics and artificial intelligence for predicting response to neoadjuvant drug therapy in patients with breast cancer: a review
Resumo
Breast cancer remains one of the most pressing challenges in modern oncology and is the most common malignant neoplasm among women worldwide. Breast cancer treatment requires a comprehensive approach, including surgery, chemotherapy, radiation therapy, targeted therapy, and hormone therapy. A particularly important role in current clinical practice belongs to neoadjuvant therapy—an approach administered prior to surgery, aimed at reducing tumor size, increasing the likelihood of breast-conserving surgery, and evaluating the tumor’s individual sensitivity to drug therapy. Neoadjuvant therapy is the standard of care for locally advanced, initially inoperable invasive breast cancer. It is also recommended as a first-line treatment for patients with initially operable but biologically aggressive tumor subtypes, such as triple-negative and HER2-positive breast cancer. However, individual responses to therapy vary significantly: some patients demonstrate a good response to neoadjuvant treatment, which markedly improves their prognosis, whereas in others the treatment may prove ineffective. Early prediction of therapeutic response to neoadjuvant treatment helps to avoid unnecessary drug dose exposure, reduce the financial burden on the healthcare system, and minimize the risk of adverse effects. In recent years, radiomics and artificial intelligence methods have been actively developed to analyze medical imaging and detect hidden biomarkers associated with treatment response. This review analyzes articles from recent decades in which diverse prognostic models were developed to evaluate neoadjuvant treatment response through the application of radiomics and artificial intelligence methods. Special attention is given to papers demonstrating the potential of machine learning and deep data analysis aimed at personalizing breast cancer therapy. These innovative approaches offer new opportunities for improving treatment effectiveness and patient survival.
 331-344
331-344


Editorials
Good publication practices: declaration, approval, and now enforcement of reporting standards
Resumo
This article introduces a new submission policy for original research manuscripts. Starting next year, such manuscripts will be considered only if they comply with the reporting guidelines recommended by the EQUATOR (Enhancing the QUAlity and Transparency Of health Research) Network and are approved by an ethics committee during the planning stage. The information to be included in a manuscript upon submission has been expanded. When these rules are fully implemented, prior study registration and submission of primary research data to the editorial office (with subsequent publication upon article acceptance) will become mandatory for manuscript consideration. These changes aim to transition the journal from organic growth to controlled development according to the principles of scientific integrity.
 345-355
345-355